A Complication of a Retropharyngeal Abscess
Radiology Cases in Pediatric Emergency Medicine
Volume 7, Case 10
Orn-Usa Lisa Boonprakong, Medical Student
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is an 8 month old male who was in his usual
state of health until 2 weeks ago when he developed
fever (38 to 39 degrees C), intermittent cough,
congestion, and increased secretions. He was treated
with antibiotics by his primary care physician. One
week ago, he developed hives with wheezing, stridor
and tachypnea. He was treated with albuterol and
prednisolone with subsequent relief. Three days ago,
he then developed a dry cough, shallow respirations,
and apparent stiffness of his neck with an inability to
straighten his neck or bring his head to midline. He
was most comfortable in the position of being upright or
lying on his side. Gradually, his respirations became
"noisy and gurgly". He now presents to a rural
emergency department with worsening stridor. His past
medical history is unremarkable.
Exam: VS T39, P120, R40, oxygen saturation
98-100% on RA. He is somewhat irritable but easily
arousable and consolable, holding his neck in a solitary
position. Eyes normal. Nares are clear without
drainage. Tympanic membranes normal. His oral
cavity is clear, with moist mucosa. The posterior
pharynx is very full, with slightly enlarged tonsils
bilaterally. His neck is slightly stiff with discomfort
experienced on movement. There is right-sided
cervical lymphadenopathy, with slight tracheal
deviation to the right. Breath sounds demonstrate
moderate stridor with slight coarse rhonchi. Heart
regular rate and rhythm, without murmur. Abdomen is
soft and flat, normal bowel sounds, no organomegaly.
His extremities are warm with normal capillary refill.
His skin demonstrates no rashes or lesions.
Radiographs of his chest and neck are ordered.
Can you identify the abnormalities on his radiographs.
View his chest and lateral neck radiographs.
His chest radiographs
 His lateral neck radiograph
His lateral neck radiograph
 His lateral neck radiograph shows severe
prevertebral soft tissue swelling with extension
inferiorly. The width of the prevertebral soft tissue
should normally be about half the width of a vertebral
body (see Case 10 of Volume 1). In this case, it is very
wide. His chest radiograph demonstrates a widened
mediastinum and shift of the airway to the right.
He is intubated using rapid sequence intubation to
ensure a stable airway during air transport to a
children's hospital for further management. A CT scan
of the chest is obtained prior to transport.
View his chest CT scan.
His lateral neck radiograph shows severe
prevertebral soft tissue swelling with extension
inferiorly. The width of the prevertebral soft tissue
should normally be about half the width of a vertebral
body (see Case 10 of Volume 1). In this case, it is very
wide. His chest radiograph demonstrates a widened
mediastinum and shift of the airway to the right.
He is intubated using rapid sequence intubation to
ensure a stable airway during air transport to a
children's hospital for further management. A CT scan
of the chest is obtained prior to transport.
View his chest CT scan.
 Scout view showing image cut levels
Scout view showing image cut levels
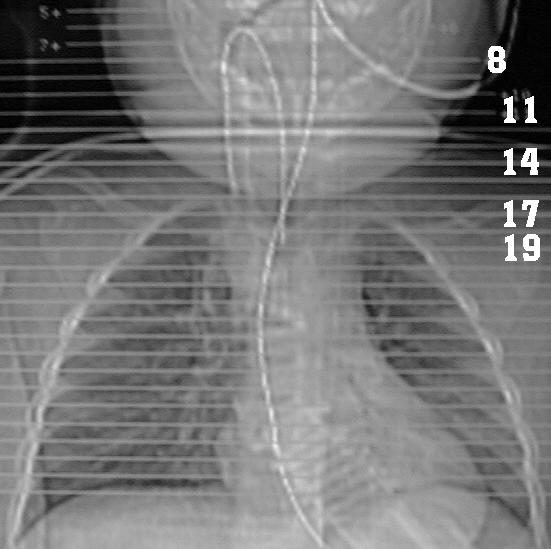 The CT scan demonstrates a retropharyngeal
abscess that extends towards the posterior
mediastinum to the level of the aortic arch. This image
shows the abscess (black arrows) on cuts 8, 11, 14, 17
and 19 from his CT study. The level of these cuts are
demonstrated on the scout view. At a level
through his mouth, cut 8 shows the large abscess
cavity which bulges anteriorly. At chin level, cut 11
shows the abscess with a typical enhancing rim. Cut
14 shows the abscess at mid-neck level. Cut 17 shows
extension of the abscess into the mediastinum at the
level of the lung apices. Cut 19 shows extension of the
abscess into the mediastinum at the level of the upper
lobes.
He was initially placed on clindamycin and
cefotaxime. He underwent a surgical drainage
procedure for both the retropharyngeal and mediastinal
abscesses. Cultures of the pus grew Group A beta
hemolytic streptococci, at which time he was changed
to penicillin.
Discussion
The retropharyngeal space is a potential space in
the deep neck that is bordered by the buccopharyngeal
fascia anteriorly, the prevertebral fascia posteriorly,
and the carotid sheath laterally. An infection
developing in this space could potentially spread into
the mediastinum and other deep neck compartments.
In the pediatric population, this space contains lymph
nodes draining the nasopharynx, paranasal sinuses,
nasal cavity, and soft palate. These retropharyngeal
nodes atrophy at puberty making abscess formation
less likely in teens and adults.
Retropharyngeal abscesses are most commonly
present in children less than 3 years of age. In the
pediatric population, retropharyngeal abscesses
typically result from upper respiratory infections
(particularly oropharyngeal infections) with suppurative
cervical lymphadenopathy, whereas in adults they
normally occur secondary to trauma to the oropharynx,
iatrogenic instrumentation, foreign bodies, or dental
infections.
Initial antimicrobial empiric therapy is directed
towards the aerobic and anaerobic flora of the
nasopharynx. Common aerobes are Staphylococcus
aureas, alpha hemolytic and non-hemolytic
streptococci, Haemophilus species, and group A
beta-hemolytic Streptococci. Common anaerobes are
bacteriodes, peptostreptococci, and fusobacteria.
During surgical drainage, an aspirate of the pus is
obtained for specific determination of the causative
microorganism(s).
Signs and symptoms include high fever, dysphagia,
odynophagia, drooling, neck/cervical rigidity and
swelling, anorexia, a "hot potato"/muffled voice,
bulging/fluctuance of the posterior pharyngeal wall
which is usually difficult to see. Dysphagia and
drooling are more common indicators of actual upper
airway involvement, whereas inspiratory stridor is less
common.
When suspected clinically, a lateral neck radiograph
is usually adequate to diagnose the presence of a
retropharyngeal abscess. A true lateral neck x-ray
should be taken in extension (cervical spine lordosis
should be visible on the radiograph) and inspiration.
The anteroposterior diameter of the prevertebral soft
tissues should not exceed the width of the vertebral
bodies. With a retropharyngeal abscess, a classic
widened soft tissue shadow anterior to the cervical
vertebrae is seen with a normal epiglottis and
aryepiglottic folds.
A CT scan is diagnostically useful to distinguish
between abscess (requiring surgical drainage) and a
phlegmon cellulitis (which may not require surgical
drainage), indicating the extent of abscess involvement,
localizing the lesion prior to surgical intervention, and
to differentiate which deep neck spaces are involved
(see Case 1 of Volume 5).
Retropharyngeal abscess is in the differential
diagnosis of a febrile infant with airway obstruction.
Usually a high index of suspicion is needed to identify a
child with a retropharyngeal abscess. The presentation
of a stiff neck can initially be misdiagnosed as
meningitis, and inspiratory stridor may mimic croup or
epiglottitis.
Treatment of a retropharyngeal abscess requiers
the maintainance of a stable airway, thus, endotracheal
intubation may be necessary if airway compromise is
present. IV antibiotics are required. Surgical drainage
is usually required in a true abscess. Perioral drainage
is normally adequate for uncomplicated infections that
have not entered other deep neck spaces or affected
the airway. External drainage, along the anterior
aspect of the sternocleidomastoid, between the carotid
sheath and inferior constrictor muscle, is usually
required for the more severe infections that have
spread to other compartments. Antibiotics should
initially cover the common microbes (i.e. streptococci,
staph aureus, anaerobes).
Complications include mediastinitis and mediastinal
abscess secondary to spread from the retropharyngeal
space (being contiguous with the mediastinum), airway
obstruction, and rupture of the abscess with potential
aspiration of pus and pneumonia. Mediastinitis is a
rare and life-threatening complication with a mortality
rate as high as 40%. Most cases of reported
suppurative mediastinitis have been secondary to
esophageal perforation (traumatic or nontraumatic) and
after median sternotomy.
When managing a patient with a retropharyngeal
abscess, physicians should consider the possibility of
this complication. Chest radiographs may be
necessary to rule out mediastinal or pulmonary
involvement. A CT scan will also be helpful in
determining the extent of the abscess. The extension
of the infection of the neck to the mediastinum has
been attributed to synergistic necrotizing bacterial
growth, negative intrathoracic pressure, and dependent
drainage from the neck to the mediastinum. The high
occurrence of mixed aerobic and anaerobic flora in
retropharyngeal abscess complicated by mediastinitis
may account for the necrotizing nature of this type of
infection. Immediate diagnosis and surgical drainage
of the retropharyngeal and mediastinal abscesses are
essential for treatment.
References
1. Gaglani MJ, Morven SE. Clinical Indicators of
Childhood Retropharyngeal Abscess. Am J Emerg Med
1995;13(3):333-335.
2. Goldenerg D, Gotz A, Joachms HZ.
Retropharyngeal Abscess: a Clinical Review. J
Laryngol Otol 1997;111:546-550.
3. Lalakea ML, Messner AH. Retropharyngeal
Abscess Management in Children: Current Practices.
Otolaryngol Head Neck Surg 1999;121(4):398-405.
4. Sztajnbok J, Grassi MS, Katayama DM, Troster
EJ. Descending Suppurative Mediastinitis: Nonsurgical
Approach to this Unusual Complication of
Retropharyngeal Abscesses in Childhood. Pediatr
Emerg Care 1999;15(5):341-343.
The CT scan demonstrates a retropharyngeal
abscess that extends towards the posterior
mediastinum to the level of the aortic arch. This image
shows the abscess (black arrows) on cuts 8, 11, 14, 17
and 19 from his CT study. The level of these cuts are
demonstrated on the scout view. At a level
through his mouth, cut 8 shows the large abscess
cavity which bulges anteriorly. At chin level, cut 11
shows the abscess with a typical enhancing rim. Cut
14 shows the abscess at mid-neck level. Cut 17 shows
extension of the abscess into the mediastinum at the
level of the lung apices. Cut 19 shows extension of the
abscess into the mediastinum at the level of the upper
lobes.
He was initially placed on clindamycin and
cefotaxime. He underwent a surgical drainage
procedure for both the retropharyngeal and mediastinal
abscesses. Cultures of the pus grew Group A beta
hemolytic streptococci, at which time he was changed
to penicillin.
Discussion
The retropharyngeal space is a potential space in
the deep neck that is bordered by the buccopharyngeal
fascia anteriorly, the prevertebral fascia posteriorly,
and the carotid sheath laterally. An infection
developing in this space could potentially spread into
the mediastinum and other deep neck compartments.
In the pediatric population, this space contains lymph
nodes draining the nasopharynx, paranasal sinuses,
nasal cavity, and soft palate. These retropharyngeal
nodes atrophy at puberty making abscess formation
less likely in teens and adults.
Retropharyngeal abscesses are most commonly
present in children less than 3 years of age. In the
pediatric population, retropharyngeal abscesses
typically result from upper respiratory infections
(particularly oropharyngeal infections) with suppurative
cervical lymphadenopathy, whereas in adults they
normally occur secondary to trauma to the oropharynx,
iatrogenic instrumentation, foreign bodies, or dental
infections.
Initial antimicrobial empiric therapy is directed
towards the aerobic and anaerobic flora of the
nasopharynx. Common aerobes are Staphylococcus
aureas, alpha hemolytic and non-hemolytic
streptococci, Haemophilus species, and group A
beta-hemolytic Streptococci. Common anaerobes are
bacteriodes, peptostreptococci, and fusobacteria.
During surgical drainage, an aspirate of the pus is
obtained for specific determination of the causative
microorganism(s).
Signs and symptoms include high fever, dysphagia,
odynophagia, drooling, neck/cervical rigidity and
swelling, anorexia, a "hot potato"/muffled voice,
bulging/fluctuance of the posterior pharyngeal wall
which is usually difficult to see. Dysphagia and
drooling are more common indicators of actual upper
airway involvement, whereas inspiratory stridor is less
common.
When suspected clinically, a lateral neck radiograph
is usually adequate to diagnose the presence of a
retropharyngeal abscess. A true lateral neck x-ray
should be taken in extension (cervical spine lordosis
should be visible on the radiograph) and inspiration.
The anteroposterior diameter of the prevertebral soft
tissues should not exceed the width of the vertebral
bodies. With a retropharyngeal abscess, a classic
widened soft tissue shadow anterior to the cervical
vertebrae is seen with a normal epiglottis and
aryepiglottic folds.
A CT scan is diagnostically useful to distinguish
between abscess (requiring surgical drainage) and a
phlegmon cellulitis (which may not require surgical
drainage), indicating the extent of abscess involvement,
localizing the lesion prior to surgical intervention, and
to differentiate which deep neck spaces are involved
(see Case 1 of Volume 5).
Retropharyngeal abscess is in the differential
diagnosis of a febrile infant with airway obstruction.
Usually a high index of suspicion is needed to identify a
child with a retropharyngeal abscess. The presentation
of a stiff neck can initially be misdiagnosed as
meningitis, and inspiratory stridor may mimic croup or
epiglottitis.
Treatment of a retropharyngeal abscess requiers
the maintainance of a stable airway, thus, endotracheal
intubation may be necessary if airway compromise is
present. IV antibiotics are required. Surgical drainage
is usually required in a true abscess. Perioral drainage
is normally adequate for uncomplicated infections that
have not entered other deep neck spaces or affected
the airway. External drainage, along the anterior
aspect of the sternocleidomastoid, between the carotid
sheath and inferior constrictor muscle, is usually
required for the more severe infections that have
spread to other compartments. Antibiotics should
initially cover the common microbes (i.e. streptococci,
staph aureus, anaerobes).
Complications include mediastinitis and mediastinal
abscess secondary to spread from the retropharyngeal
space (being contiguous with the mediastinum), airway
obstruction, and rupture of the abscess with potential
aspiration of pus and pneumonia. Mediastinitis is a
rare and life-threatening complication with a mortality
rate as high as 40%. Most cases of reported
suppurative mediastinitis have been secondary to
esophageal perforation (traumatic or nontraumatic) and
after median sternotomy.
When managing a patient with a retropharyngeal
abscess, physicians should consider the possibility of
this complication. Chest radiographs may be
necessary to rule out mediastinal or pulmonary
involvement. A CT scan will also be helpful in
determining the extent of the abscess. The extension
of the infection of the neck to the mediastinum has
been attributed to synergistic necrotizing bacterial
growth, negative intrathoracic pressure, and dependent
drainage from the neck to the mediastinum. The high
occurrence of mixed aerobic and anaerobic flora in
retropharyngeal abscess complicated by mediastinitis
may account for the necrotizing nature of this type of
infection. Immediate diagnosis and surgical drainage
of the retropharyngeal and mediastinal abscesses are
essential for treatment.
References
1. Gaglani MJ, Morven SE. Clinical Indicators of
Childhood Retropharyngeal Abscess. Am J Emerg Med
1995;13(3):333-335.
2. Goldenerg D, Gotz A, Joachms HZ.
Retropharyngeal Abscess: a Clinical Review. J
Laryngol Otol 1997;111:546-550.
3. Lalakea ML, Messner AH. Retropharyngeal
Abscess Management in Children: Current Practices.
Otolaryngol Head Neck Surg 1999;121(4):398-405.
4. Sztajnbok J, Grassi MS, Katayama DM, Troster
EJ. Descending Suppurative Mediastinitis: Nonsurgical
Approach to this Unusual Complication of
Retropharyngeal Abscesses in Childhood. Pediatr
Emerg Care 1999;15(5):341-343.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 His lateral neck radiograph
His lateral neck radiograph
 His lateral neck radiograph shows severe
prevertebral soft tissue swelling with extension
inferiorly. The width of the prevertebral soft tissue
should normally be about half the width of a vertebral
body (see Case 10 of Volume 1). In this case, it is very
wide. His chest radiograph demonstrates a widened
mediastinum and shift of the airway to the right.
He is intubated using rapid sequence intubation to
ensure a stable airway during air transport to a
children's hospital for further management. A CT scan
of the chest is obtained prior to transport.
View his chest CT scan.
His lateral neck radiograph shows severe
prevertebral soft tissue swelling with extension
inferiorly. The width of the prevertebral soft tissue
should normally be about half the width of a vertebral
body (see Case 10 of Volume 1). In this case, it is very
wide. His chest radiograph demonstrates a widened
mediastinum and shift of the airway to the right.
He is intubated using rapid sequence intubation to
ensure a stable airway during air transport to a
children's hospital for further management. A CT scan
of the chest is obtained prior to transport.
View his chest CT scan.
 Scout view showing image cut levels
Scout view showing image cut levels
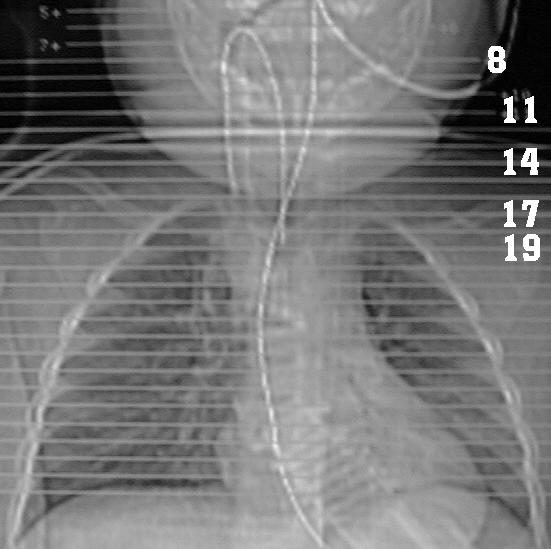 The CT scan demonstrates a retropharyngeal
abscess that extends towards the posterior
mediastinum to the level of the aortic arch. This image
shows the abscess (black arrows) on cuts 8, 11, 14, 17
and 19 from his CT study. The level of these cuts are
demonstrated on the scout view. At a level
through his mouth, cut 8 shows the large abscess
cavity which bulges anteriorly. At chin level, cut 11
shows the abscess with a typical enhancing rim. Cut
14 shows the abscess at mid-neck level. Cut 17 shows
extension of the abscess into the mediastinum at the
level of the lung apices. Cut 19 shows extension of the
abscess into the mediastinum at the level of the upper
lobes.
He was initially placed on clindamycin and
cefotaxime. He underwent a surgical drainage
procedure for both the retropharyngeal and mediastinal
abscesses. Cultures of the pus grew Group A beta
hemolytic streptococci, at which time he was changed
to penicillin.
Discussion
The retropharyngeal space is a potential space in
the deep neck that is bordered by the buccopharyngeal
fascia anteriorly, the prevertebral fascia posteriorly,
and the carotid sheath laterally. An infection
developing in this space could potentially spread into
the mediastinum and other deep neck compartments.
In the pediatric population, this space contains lymph
nodes draining the nasopharynx, paranasal sinuses,
nasal cavity, and soft palate. These retropharyngeal
nodes atrophy at puberty making abscess formation
less likely in teens and adults.
Retropharyngeal abscesses are most commonly
present in children less than 3 years of age. In the
pediatric population, retropharyngeal abscesses
typically result from upper respiratory infections
(particularly oropharyngeal infections) with suppurative
cervical lymphadenopathy, whereas in adults they
normally occur secondary to trauma to the oropharynx,
iatrogenic instrumentation, foreign bodies, or dental
infections.
Initial antimicrobial empiric therapy is directed
towards the aerobic and anaerobic flora of the
nasopharynx. Common aerobes are Staphylococcus
aureas, alpha hemolytic and non-hemolytic
streptococci, Haemophilus species, and group A
beta-hemolytic Streptococci. Common anaerobes are
bacteriodes, peptostreptococci, and fusobacteria.
During surgical drainage, an aspirate of the pus is
obtained for specific determination of the causative
microorganism(s).
Signs and symptoms include high fever, dysphagia,
odynophagia, drooling, neck/cervical rigidity and
swelling, anorexia, a "hot potato"/muffled voice,
bulging/fluctuance of the posterior pharyngeal wall
which is usually difficult to see. Dysphagia and
drooling are more common indicators of actual upper
airway involvement, whereas inspiratory stridor is less
common.
When suspected clinically, a lateral neck radiograph
is usually adequate to diagnose the presence of a
retropharyngeal abscess. A true lateral neck x-ray
should be taken in extension (cervical spine lordosis
should be visible on the radiograph) and inspiration.
The anteroposterior diameter of the prevertebral soft
tissues should not exceed the width of the vertebral
bodies. With a retropharyngeal abscess, a classic
widened soft tissue shadow anterior to the cervical
vertebrae is seen with a normal epiglottis and
aryepiglottic folds.
A CT scan is diagnostically useful to distinguish
between abscess (requiring surgical drainage) and a
phlegmon cellulitis (which may not require surgical
drainage), indicating the extent of abscess involvement,
localizing the lesion prior to surgical intervention, and
to differentiate which deep neck spaces are involved
(see Case 1 of Volume 5).
Retropharyngeal abscess is in the differential
diagnosis of a febrile infant with airway obstruction.
Usually a high index of suspicion is needed to identify a
child with a retropharyngeal abscess. The presentation
of a stiff neck can initially be misdiagnosed as
meningitis, and inspiratory stridor may mimic croup or
epiglottitis.
Treatment of a retropharyngeal abscess requiers
the maintainance of a stable airway, thus, endotracheal
intubation may be necessary if airway compromise is
present. IV antibiotics are required. Surgical drainage
is usually required in a true abscess. Perioral drainage
is normally adequate for uncomplicated infections that
have not entered other deep neck spaces or affected
the airway. External drainage, along the anterior
aspect of the sternocleidomastoid, between the carotid
sheath and inferior constrictor muscle, is usually
required for the more severe infections that have
spread to other compartments. Antibiotics should
initially cover the common microbes (i.e. streptococci,
staph aureus, anaerobes).
Complications include mediastinitis and mediastinal
abscess secondary to spread from the retropharyngeal
space (being contiguous with the mediastinum), airway
obstruction, and rupture of the abscess with potential
aspiration of pus and pneumonia. Mediastinitis is a
rare and life-threatening complication with a mortality
rate as high as 40%. Most cases of reported
suppurative mediastinitis have been secondary to
esophageal perforation (traumatic or nontraumatic) and
after median sternotomy.
When managing a patient with a retropharyngeal
abscess, physicians should consider the possibility of
this complication. Chest radiographs may be
necessary to rule out mediastinal or pulmonary
involvement. A CT scan will also be helpful in
determining the extent of the abscess. The extension
of the infection of the neck to the mediastinum has
been attributed to synergistic necrotizing bacterial
growth, negative intrathoracic pressure, and dependent
drainage from the neck to the mediastinum. The high
occurrence of mixed aerobic and anaerobic flora in
retropharyngeal abscess complicated by mediastinitis
may account for the necrotizing nature of this type of
infection. Immediate diagnosis and surgical drainage
of the retropharyngeal and mediastinal abscesses are
essential for treatment.
References
1. Gaglani MJ, Morven SE. Clinical Indicators of
Childhood Retropharyngeal Abscess. Am J Emerg Med
1995;13(3):333-335.
2. Goldenerg D, Gotz A, Joachms HZ.
Retropharyngeal Abscess: a Clinical Review. J
Laryngol Otol 1997;111:546-550.
3. Lalakea ML, Messner AH. Retropharyngeal
Abscess Management in Children: Current Practices.
Otolaryngol Head Neck Surg 1999;121(4):398-405.
4. Sztajnbok J, Grassi MS, Katayama DM, Troster
EJ. Descending Suppurative Mediastinitis: Nonsurgical
Approach to this Unusual Complication of
Retropharyngeal Abscesses in Childhood. Pediatr
Emerg Care 1999;15(5):341-343.
The CT scan demonstrates a retropharyngeal
abscess that extends towards the posterior
mediastinum to the level of the aortic arch. This image
shows the abscess (black arrows) on cuts 8, 11, 14, 17
and 19 from his CT study. The level of these cuts are
demonstrated on the scout view. At a level
through his mouth, cut 8 shows the large abscess
cavity which bulges anteriorly. At chin level, cut 11
shows the abscess with a typical enhancing rim. Cut
14 shows the abscess at mid-neck level. Cut 17 shows
extension of the abscess into the mediastinum at the
level of the lung apices. Cut 19 shows extension of the
abscess into the mediastinum at the level of the upper
lobes.
He was initially placed on clindamycin and
cefotaxime. He underwent a surgical drainage
procedure for both the retropharyngeal and mediastinal
abscesses. Cultures of the pus grew Group A beta
hemolytic streptococci, at which time he was changed
to penicillin.
Discussion
The retropharyngeal space is a potential space in
the deep neck that is bordered by the buccopharyngeal
fascia anteriorly, the prevertebral fascia posteriorly,
and the carotid sheath laterally. An infection
developing in this space could potentially spread into
the mediastinum and other deep neck compartments.
In the pediatric population, this space contains lymph
nodes draining the nasopharynx, paranasal sinuses,
nasal cavity, and soft palate. These retropharyngeal
nodes atrophy at puberty making abscess formation
less likely in teens and adults.
Retropharyngeal abscesses are most commonly
present in children less than 3 years of age. In the
pediatric population, retropharyngeal abscesses
typically result from upper respiratory infections
(particularly oropharyngeal infections) with suppurative
cervical lymphadenopathy, whereas in adults they
normally occur secondary to trauma to the oropharynx,
iatrogenic instrumentation, foreign bodies, or dental
infections.
Initial antimicrobial empiric therapy is directed
towards the aerobic and anaerobic flora of the
nasopharynx. Common aerobes are Staphylococcus
aureas, alpha hemolytic and non-hemolytic
streptococci, Haemophilus species, and group A
beta-hemolytic Streptococci. Common anaerobes are
bacteriodes, peptostreptococci, and fusobacteria.
During surgical drainage, an aspirate of the pus is
obtained for specific determination of the causative
microorganism(s).
Signs and symptoms include high fever, dysphagia,
odynophagia, drooling, neck/cervical rigidity and
swelling, anorexia, a "hot potato"/muffled voice,
bulging/fluctuance of the posterior pharyngeal wall
which is usually difficult to see. Dysphagia and
drooling are more common indicators of actual upper
airway involvement, whereas inspiratory stridor is less
common.
When suspected clinically, a lateral neck radiograph
is usually adequate to diagnose the presence of a
retropharyngeal abscess. A true lateral neck x-ray
should be taken in extension (cervical spine lordosis
should be visible on the radiograph) and inspiration.
The anteroposterior diameter of the prevertebral soft
tissues should not exceed the width of the vertebral
bodies. With a retropharyngeal abscess, a classic
widened soft tissue shadow anterior to the cervical
vertebrae is seen with a normal epiglottis and
aryepiglottic folds.
A CT scan is diagnostically useful to distinguish
between abscess (requiring surgical drainage) and a
phlegmon cellulitis (which may not require surgical
drainage), indicating the extent of abscess involvement,
localizing the lesion prior to surgical intervention, and
to differentiate which deep neck spaces are involved
(see Case 1 of Volume 5).
Retropharyngeal abscess is in the differential
diagnosis of a febrile infant with airway obstruction.
Usually a high index of suspicion is needed to identify a
child with a retropharyngeal abscess. The presentation
of a stiff neck can initially be misdiagnosed as
meningitis, and inspiratory stridor may mimic croup or
epiglottitis.
Treatment of a retropharyngeal abscess requiers
the maintainance of a stable airway, thus, endotracheal
intubation may be necessary if airway compromise is
present. IV antibiotics are required. Surgical drainage
is usually required in a true abscess. Perioral drainage
is normally adequate for uncomplicated infections that
have not entered other deep neck spaces or affected
the airway. External drainage, along the anterior
aspect of the sternocleidomastoid, between the carotid
sheath and inferior constrictor muscle, is usually
required for the more severe infections that have
spread to other compartments. Antibiotics should
initially cover the common microbes (i.e. streptococci,
staph aureus, anaerobes).
Complications include mediastinitis and mediastinal
abscess secondary to spread from the retropharyngeal
space (being contiguous with the mediastinum), airway
obstruction, and rupture of the abscess with potential
aspiration of pus and pneumonia. Mediastinitis is a
rare and life-threatening complication with a mortality
rate as high as 40%. Most cases of reported
suppurative mediastinitis have been secondary to
esophageal perforation (traumatic or nontraumatic) and
after median sternotomy.
When managing a patient with a retropharyngeal
abscess, physicians should consider the possibility of
this complication. Chest radiographs may be
necessary to rule out mediastinal or pulmonary
involvement. A CT scan will also be helpful in
determining the extent of the abscess. The extension
of the infection of the neck to the mediastinum has
been attributed to synergistic necrotizing bacterial
growth, negative intrathoracic pressure, and dependent
drainage from the neck to the mediastinum. The high
occurrence of mixed aerobic and anaerobic flora in
retropharyngeal abscess complicated by mediastinitis
may account for the necrotizing nature of this type of
infection. Immediate diagnosis and surgical drainage
of the retropharyngeal and mediastinal abscesses are
essential for treatment.
References
1. Gaglani MJ, Morven SE. Clinical Indicators of
Childhood Retropharyngeal Abscess. Am J Emerg Med
1995;13(3):333-335.
2. Goldenerg D, Gotz A, Joachms HZ.
Retropharyngeal Abscess: a Clinical Review. J
Laryngol Otol 1997;111:546-550.
3. Lalakea ML, Messner AH. Retropharyngeal
Abscess Management in Children: Current Practices.
Otolaryngol Head Neck Surg 1999;121(4):398-405.
4. Sztajnbok J, Grassi MS, Katayama DM, Troster
EJ. Descending Suppurative Mediastinitis: Nonsurgical
Approach to this Unusual Complication of
Retropharyngeal Abscesses in Childhood. Pediatr
Emerg Care 1999;15(5):341-343.