Orbital Pseudotumor
Radiology Cases in Pediatric Emergency Medicine
Volume 6, Case 10
Martin I. Herman, MD
LeBonheur Children's Medical Center
University of Tennessee School of Medicine
This is a 2 year old male who presents with a chief
complaint of bilateral eye swelling. He had some
swelling noted 2 weeks prior to this admission and was
treated with antibiotics for a presumed sinusitis. The
swelling did improve to some degree; however it never
completely resolved. Over the past 2 weeks the
swelling has worsened. There has been some itching
but no fever. His vision is unaffected as far as his
mother could tell. Diphenhydramine and erythromycin
ophthalmic ointment were started and once again the
swelling improved. They present today because the
swelling is again worse. Mom denied any trauma to the
lids or orbit, no eye discharge, and only mild redness.
There are no symptoms to suggest hyperthyroidism.
His past medical history is negative for any diseases
of the eyes, severe allergies, renal or cardiac disease,
or thyroid dysfunction. His family history is
unremarkable.
Exam. He is a healthy appearing male who has mild
proptosis of both eyes. There is mild conjunctival
erythema but no discharge. The corneas are clear. No
erythema of the lids is appreciated. Anterior chambers
are clear and extraocular movements are conjugate but
not fully testable, though the Doll's eye maneuver was
normal. There is no preauricular lymphadenopathy.
At this point, what is your working differential
diagnosis? a) non-accidental trauma, b) accidental
trauma, c) hyperthyroidism, d) periorbital or orbital
cellulitis, e) orbital malignancy (e.g., retinoblastoma), f)
other.
How would you proceed? a) visual acuity testing, b)
complete blood count, c) eye culture, d) ophthalmology
consult, e) all of the above.
Answer: e) all of the above. Culture of the eye
discharge or conjunctiva is needed to rule out bacterial
conjunctivitis. Blood work for thyroid function and
complete blood count (CBC) is useful to check for other
etiologies of the proptosis and for the possibility of
hematologic malignancy. Visual acuity testing should
be done in every case of symptoms related to the eye.
Ophthalmology is needed because of the possibility that
surgical intervention my be indicated.
His visual acuity is probably normal, but this is
difficult to test well in a 2 year old. His CBC is normal
and eye cultures were obtained. An ophthalmology
consult was obtained and a CT of the orbits is ordered.
View CT scan.
 What does the CT show? Does this alter your
differential? What should be done now?
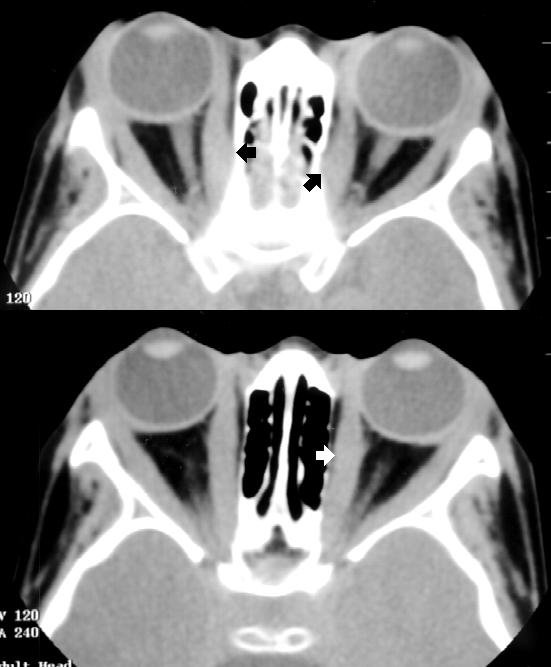
The CT of this child's orbits reveals thickening of the
orbital structures. Thickening/swelling of the
extraocular muscles is most evident. No calcifications
are noted. The globes are normal and no bony
erosions are noted. The remainder of the study is
normal. These findings are consistent with orbital
pseudotumor.
What does the CT show? Does this alter your
differential? What should be done now?
The CT of this child's orbits reveals thickening of the
orbital structures. Thickening/swelling of the
extraocular muscles is most evident. No calcifications
are noted. The globes are normal and no bony
erosions are noted. The remainder of the study is
normal. These findings are consistent with orbital
pseudotumor.
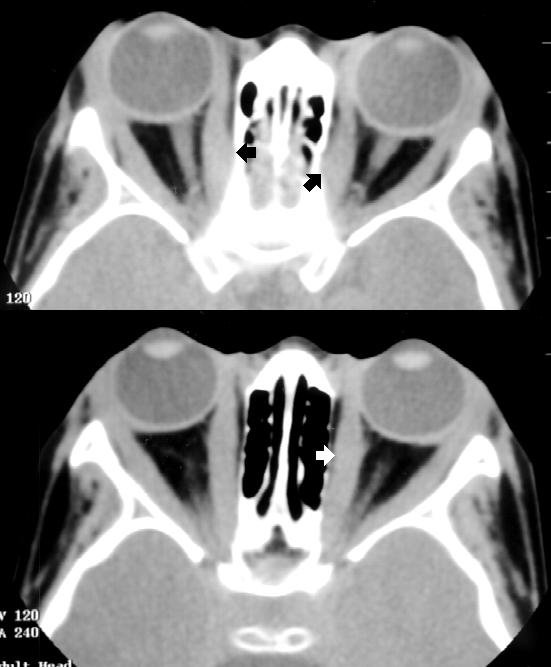 The arrows here point to the enlarged extraocular
muscles resulting in anterior displacement of the globe.
Although the arrows point fo just some of the lateral and
medial rectus muscles, ALL the extraocular muscles are
enlarged.
Discussion:
Orbital pseudotumor (OP) or idiopathic non-specific
orbital inflammation is a non-infectious acute
inflammation of the orbits, that presents with orbital
swelling or a mass. It is usually unilateral, but it may be
bilateral as it was in this case. It is uncommon in
children but it has been reported in children as young
as 3 months of age. OP may present as proptosis, eye
pain, ptosis, lid edema, conjunctivitis with or without
chemosis (swelling of the conjunctiva) and limitation of
extraocular movements. Fever, headaches and eye
discharge may be found. Orbital involvement is
generally unilateral and recurrences may occur.
Sometimes one can palpate a mass above the temple
or under the orbital rim. Autoimmune disorders have
been associated with this condition. The differential
diagnosis includes orbital cellulitis, orbital abscess,
tuberculoma, hematoma, inflammation secondary to
systemic disease such as Grave's disease, sarcoidosis,
a retained foreign body, leukemia, lymphoma, optic
neuritis, tumors (primary, metastatic and pseudo).
To establish a diagnosis, ultrasonography and/or
CT of the orbits is often necessary. Special laboratory
studies such as markers for rheumatoid disease or
thyroid dysfunction may also be helpful. The CT
typically demonstrates diffuse anterior orbital
inflammation next to the globe with scleral and
choroidal thickening. Enlargement of the extraocular
muscles may also be seen on either ultrasound or CT
scan.
After an imaging diagnosis is made, a biopsy may
be necessary to rule out leukemia or lymphoma. The
histopathology of orbital pseudotumor shows
polymorphic lymphocytic and plasmacytic infiltrates with
eosinophilia. Corticosteroids are the mainstay of
therapy. Once started, the symptoms quickly resolve
as they did in our case. In fact, the response to
steroids is so pathognomonic, that the diagnosis is
often made retrospectively based on the response. A
poor response indicates the need for biopsy.
References
Grossniklaus HE, Lass JH, Abramowsky CR, Levine
MR. Childhood orbital pseudotumor. Ann Opthalmol
1985;17(6):372-377.
Sirbaugh PE. A case of orbital pseudotumor
masquerading as orbital cellulitis in a patient with
proptosis and fever. Ped Emerg Care
1997;13(5):337-339.
The arrows here point to the enlarged extraocular
muscles resulting in anterior displacement of the globe.
Although the arrows point fo just some of the lateral and
medial rectus muscles, ALL the extraocular muscles are
enlarged.
Discussion:
Orbital pseudotumor (OP) or idiopathic non-specific
orbital inflammation is a non-infectious acute
inflammation of the orbits, that presents with orbital
swelling or a mass. It is usually unilateral, but it may be
bilateral as it was in this case. It is uncommon in
children but it has been reported in children as young
as 3 months of age. OP may present as proptosis, eye
pain, ptosis, lid edema, conjunctivitis with or without
chemosis (swelling of the conjunctiva) and limitation of
extraocular movements. Fever, headaches and eye
discharge may be found. Orbital involvement is
generally unilateral and recurrences may occur.
Sometimes one can palpate a mass above the temple
or under the orbital rim. Autoimmune disorders have
been associated with this condition. The differential
diagnosis includes orbital cellulitis, orbital abscess,
tuberculoma, hematoma, inflammation secondary to
systemic disease such as Grave's disease, sarcoidosis,
a retained foreign body, leukemia, lymphoma, optic
neuritis, tumors (primary, metastatic and pseudo).
To establish a diagnosis, ultrasonography and/or
CT of the orbits is often necessary. Special laboratory
studies such as markers for rheumatoid disease or
thyroid dysfunction may also be helpful. The CT
typically demonstrates diffuse anterior orbital
inflammation next to the globe with scleral and
choroidal thickening. Enlargement of the extraocular
muscles may also be seen on either ultrasound or CT
scan.
After an imaging diagnosis is made, a biopsy may
be necessary to rule out leukemia or lymphoma. The
histopathology of orbital pseudotumor shows
polymorphic lymphocytic and plasmacytic infiltrates with
eosinophilia. Corticosteroids are the mainstay of
therapy. Once started, the symptoms quickly resolve
as they did in our case. In fact, the response to
steroids is so pathognomonic, that the diagnosis is
often made retrospectively based on the response. A
poor response indicates the need for biopsy.
References
Grossniklaus HE, Lass JH, Abramowsky CR, Levine
MR. Childhood orbital pseudotumor. Ann Opthalmol
1985;17(6):372-377.
Sirbaugh PE. A case of orbital pseudotumor
masquerading as orbital cellulitis in a patient with
proptosis and fever. Ped Emerg Care
1997;13(5):337-339.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 What does the CT show? Does this alter your
differential? What should be done now?
The CT of this child's orbits reveals thickening of the
orbital structures. Thickening/swelling of the
extraocular muscles is most evident. No calcifications
are noted. The globes are normal and no bony
erosions are noted. The remainder of the study is
normal. These findings are consistent with orbital
pseudotumor.
What does the CT show? Does this alter your
differential? What should be done now?
The CT of this child's orbits reveals thickening of the
orbital structures. Thickening/swelling of the
extraocular muscles is most evident. No calcifications
are noted. The globes are normal and no bony
erosions are noted. The remainder of the study is
normal. These findings are consistent with orbital
pseudotumor.
 The arrows here point to the enlarged extraocular
muscles resulting in anterior displacement of the globe.
Although the arrows point fo just some of the lateral and
medial rectus muscles, ALL the extraocular muscles are
enlarged.
Discussion:
Orbital pseudotumor (OP) or idiopathic non-specific
orbital inflammation is a non-infectious acute
inflammation of the orbits, that presents with orbital
swelling or a mass. It is usually unilateral, but it may be
bilateral as it was in this case. It is uncommon in
children but it has been reported in children as young
as 3 months of age. OP may present as proptosis, eye
pain, ptosis, lid edema, conjunctivitis with or without
chemosis (swelling of the conjunctiva) and limitation of
extraocular movements. Fever, headaches and eye
discharge may be found. Orbital involvement is
generally unilateral and recurrences may occur.
Sometimes one can palpate a mass above the temple
or under the orbital rim. Autoimmune disorders have
been associated with this condition. The differential
diagnosis includes orbital cellulitis, orbital abscess,
tuberculoma, hematoma, inflammation secondary to
systemic disease such as Grave's disease, sarcoidosis,
a retained foreign body, leukemia, lymphoma, optic
neuritis, tumors (primary, metastatic and pseudo).
To establish a diagnosis, ultrasonography and/or
CT of the orbits is often necessary. Special laboratory
studies such as markers for rheumatoid disease or
thyroid dysfunction may also be helpful. The CT
typically demonstrates diffuse anterior orbital
inflammation next to the globe with scleral and
choroidal thickening. Enlargement of the extraocular
muscles may also be seen on either ultrasound or CT
scan.
After an imaging diagnosis is made, a biopsy may
be necessary to rule out leukemia or lymphoma. The
histopathology of orbital pseudotumor shows
polymorphic lymphocytic and plasmacytic infiltrates with
eosinophilia. Corticosteroids are the mainstay of
therapy. Once started, the symptoms quickly resolve
as they did in our case. In fact, the response to
steroids is so pathognomonic, that the diagnosis is
often made retrospectively based on the response. A
poor response indicates the need for biopsy.
References
Grossniklaus HE, Lass JH, Abramowsky CR, Levine
MR. Childhood orbital pseudotumor. Ann Opthalmol
1985;17(6):372-377.
Sirbaugh PE. A case of orbital pseudotumor
masquerading as orbital cellulitis in a patient with
proptosis and fever. Ped Emerg Care
1997;13(5):337-339.
The arrows here point to the enlarged extraocular
muscles resulting in anterior displacement of the globe.
Although the arrows point fo just some of the lateral and
medial rectus muscles, ALL the extraocular muscles are
enlarged.
Discussion:
Orbital pseudotumor (OP) or idiopathic non-specific
orbital inflammation is a non-infectious acute
inflammation of the orbits, that presents with orbital
swelling or a mass. It is usually unilateral, but it may be
bilateral as it was in this case. It is uncommon in
children but it has been reported in children as young
as 3 months of age. OP may present as proptosis, eye
pain, ptosis, lid edema, conjunctivitis with or without
chemosis (swelling of the conjunctiva) and limitation of
extraocular movements. Fever, headaches and eye
discharge may be found. Orbital involvement is
generally unilateral and recurrences may occur.
Sometimes one can palpate a mass above the temple
or under the orbital rim. Autoimmune disorders have
been associated with this condition. The differential
diagnosis includes orbital cellulitis, orbital abscess,
tuberculoma, hematoma, inflammation secondary to
systemic disease such as Grave's disease, sarcoidosis,
a retained foreign body, leukemia, lymphoma, optic
neuritis, tumors (primary, metastatic and pseudo).
To establish a diagnosis, ultrasonography and/or
CT of the orbits is often necessary. Special laboratory
studies such as markers for rheumatoid disease or
thyroid dysfunction may also be helpful. The CT
typically demonstrates diffuse anterior orbital
inflammation next to the globe with scleral and
choroidal thickening. Enlargement of the extraocular
muscles may also be seen on either ultrasound or CT
scan.
After an imaging diagnosis is made, a biopsy may
be necessary to rule out leukemia or lymphoma. The
histopathology of orbital pseudotumor shows
polymorphic lymphocytic and plasmacytic infiltrates with
eosinophilia. Corticosteroids are the mainstay of
therapy. Once started, the symptoms quickly resolve
as they did in our case. In fact, the response to
steroids is so pathognomonic, that the diagnosis is
often made retrospectively based on the response. A
poor response indicates the need for biopsy.
References
Grossniklaus HE, Lass JH, Abramowsky CR, Levine
MR. Childhood orbital pseudotumor. Ann Opthalmol
1985;17(6):372-377.
Sirbaugh PE. A case of orbital pseudotumor
masquerading as orbital cellulitis in a patient with
proptosis and fever. Ped Emerg Care
1997;13(5):337-339.