Elbow Swelling In a 2 Year Old With Liver Disease
Radiology Cases in Pediatric Emergency Medicine
Volume 6, Case 5
Donna Mendez, MD
Children's Medical Center of Dallas
University of Texas Southwestern School of Medicine
This is a 2 year old male, with a history of Alagille's
syndrome (a chronic liver condition), who presents to
the ED with elbow swelling 3 days after a fall, hitting his
head on the edge of a door. There was no loss of
consciousness or neurological symptoms. He has
normal activity and is eating and drinking as usual. He
has a one day history of a stuffy nose and cough.
There are no other complaints.
Exam: T 38.0 (tympanic). His other vital signs are
normal. He is noted to have a contusion with mild
swelling and ecchymosis over his right forehead. There
are no palpable skull deformities or areas of significant
tenderness. He is also noted to have yellow nasal
discharge, icteric sclera and a swollen right elbow with
decreased range of motion. There is no erythema,
warmth or tenderness on palpation in the area of
swelling. There is no hepatosplenomegaly, and the
remainder of the exam is unremarkable.
Because he has evidence of a systemic disease, a
CBC, ESR, CRP and a chemistry panel are ordered.
His CBC is normal. His electrolytes are normal. His
phosphorous is slightly low at 2.9 mg/dL (normal 3-6
mg/dL). His serum calcium is normal at 8.5 mg/dL. His
liver enzymes are elevated (ALT 288, AST 198, total
bilirubin 4.3, GGT 1204, alkaline phosphatase 2323
mg/dL). His ESR and CRP are normal.
Radiographs of his right elbow and forearm are
obtained.
View his forearm radiographs.
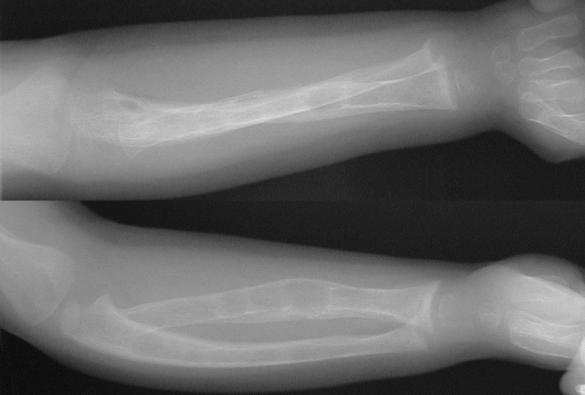 The radiograph demonstrates a healing right radial
midshaft fracture. Also noted are multiple lytic lesions
with cortical scalloping along the metaphysis and
diaphysis of the forearm bones with generalized severe
demineralization. A long bone survey is obtained.
View his lower extremity radiographs.
View femur radiographs.
The radiograph demonstrates a healing right radial
midshaft fracture. Also noted are multiple lytic lesions
with cortical scalloping along the metaphysis and
diaphysis of the forearm bones with generalized severe
demineralization. A long bone survey is obtained.
View his lower extremity radiographs.
View femur radiographs.
 View tibia radiographs.
View tibia radiographs.
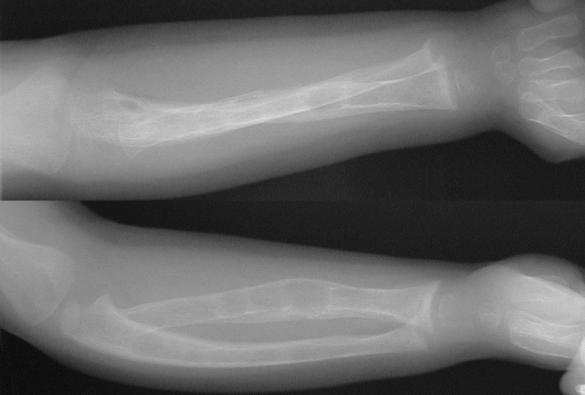
 These radiographs demonstrate epiphyseal and
metaphyseal flaring at the ends of the femur and tibia.
Lytic lesions are noted throughout the long bones.
These bony abnormalities are not primarily due to the
Alagille syndrome. What bony abnormality is present?
Teaching Points:
1) Alagille syndrome (arteriohepatic dysplasia) is
characterized by a paucity of intrahepatic bile
ducts. Clinical manifestations include chronic
cholestasis, characteristic facies, cardiovascular
abnormalities, vertebral arch defects and posterior
embryotoxin (an ocular accumulation of pigmentary
material). Cholestasis usually develops in the first few
months of life. Episodes of jaundice, are interspersed
with periods of anicteric remission. The characteristic
facies is observed in 95% of patients, consisting of a
prominent forehead, moderate hypertelorism with deep
set eyes, a small pointed chin, and a saddle or straight
nose. These features are usually not fully apparent
until 5-10 years of age.
The most common cardiovascular abnormality is
isolated and nonprogressive pulmonary stenosis of the
peripheral pulmonary vascular tree. The vertebral arch
defect seen is "butterfly-like" appearance of the dorsal
vertebrae. The accumulation of embryotoxin occurs in
more than 80% of patients with this syndrome.
Embryotoxin, a pigmentary material, accumulates in the
inner aspects of the cornea near its junction with the
iris. It is best observed with a slit lamp examination.
Other clinical manifestations include growth retardation,
renal abnormalities, mental retardation and voice
changes.
Chronic cholestasis can lead to malabsorption of fat
soluble vitamins due to lack of bile salts. Vitamin D
deficiency can result from this malabsorption as well
being due to a deficiency of 25-hydroxylation secondary
to destruction of liver parenchyma.
Diagnosis of Alagille syndrome is made by liver
biopsy and histological examination of the interlobular
bile ducts. This syndrome can be transmitted in an
autosomal dominant mode. Management includes a
high energy diet with adequate protein intake. Fat
soluble vitamins may need to be supplemented. There
is no way of predicting which patients (15%) will
progress to end stage liver disease and require
transplantation.
2) Our patient has severe demineralization and
pathologic fractures due to vitamin D deficiency
resulting in rickets. Rickets can be caused by dietary
deficiency, inadequate exposure to sunlight,
malabsorption and/or failure of metabolic activation of
vitamin D to the active form. Provitamin D3, is a
prohormone that eventually is converted to the active
form of vitamin D, 1,25-dihydroxyvitamin D3. This
active form increases intestinal calcium and
phosphorous absorption, mobilizes calcium and
phosphorous from bone to the bloodstream, and retains
calcium and phosphorous through its renal effect. This
renal effect moves calcium and phosphorous out of
older bone and also promotes the maturation and
mineralization of newly formed organic bone matrix.
In rickets, the main effect of vitamin D deficiency
results in a disorganization of the maturation and
calcification of the cartilage and its cells at the growing
ends of long bones. These abnormalities can be
correlated with radiographic findings. The widening and
lengthening of the physis represents the area of
disorganized mineralization in the zone of hypertrophy.
Widening and cupping of the metaphysis represents the
bulky mass of the hypertrophied zone placing abnormal
inward stress on the poorly mineralized metaphysis,
particularly on the more central areas.
3) The radiographic abnormalities seen in children
with rickets depend on the age of onset and duration
of illness.
a) Craniotabes: The head is particularly affected
during the first months of life. During this period, the
skull must accommodate the most rapidly growing
organ, the brain. The rapid accommodation by the skull
is associated with excess osteoid formation, particularly
at the central margins and outer table, while resorption
at the inner table continues. The thin calvarium is less
rigid and subject to supine postural influences, resulting
in posterior flattening. Continued accumulation of
osteoid in the frontal and parietal regions results in the
squared configuration known as craniotabes.
b) Long bone findings: During infancy and early
childhood, the long bones show the greatest deformity.
The metaphysis is widened, cupped and has a ragged
edge. There is a wide gap between the metaphysis and
the epiphysis corresponding to the area of disordered
mineralization. In mild cases the first radiologic sign is
a widening of the gap between the epiphysis and the
metaphysis. The characteristic bowing deformities of
the arms and legs are related to the sitting position
assumed by the child. Often, the child with severe
rickets will sit with his legs crossed. Bowing may also
result from asymmetric, musculotendinous forces that
displace the weakened growth plate. For example, the
Achilles tendon on the calcaneus displaces the distal
tibial growth plate resulting in the bowed tibia. The
shafts of long bones may also become less dense
caused by the loss of mineral content.
c) Rachitic rosary: Lumps develop at the
costochondral junctions, particularly those of the middle
ribs forming the characteristic rachitic rosary. The
costochondral junctions are the most active growth
plates and is the reason you see these changes here.
d) Harrison's groove: The distal end of the ribs are
weak and may be depressed by the negative
intrathoracic pressure developed during respiration with
a resultant semicoronal impression being found at the
costal attachment of the diaphragm, leading to the
formation of Harrison's groove.
e) Scoliosis: With increasing age, the effects of
weight bearing become prominent with scoliosis
frequently developing.
f) Looser's zones (pseudofractures): Rickets, later
in childhood, may have pseudofractures present.
Looser's zones are composed of focal accumulations of
osteoid, which is uncalcified bone matrix. They often
occur at sites where major arteries cross the bone and
have been thought to be secondary to the mechanical
stress of the pulsating vessel.
g) Fractures: Greenstick fractures of the cortex are
not uncommon.
4) Laboratory findings: In rickets, patients will have
an increased alkaline phosphatase >200, as in this
case. This is because of the active release of its stores
in bone. There are 3 stages of rickets. Stage I is the
early phase where serum calcium is low but serum
phosphorous is normal. In stage II, which occurs later,
serum calcium concentrations are restored to normal
ranges because of compensatory hyperparathyroidism,
but serum phosphorous levels are low. In stage III,
both serum calcium and phosphorous levels are low
and bone disease is florid because of the combined
effect of mineral deficiency and hyperparathyroidism.
This patient presented in stage II with a normal serum
calcium and low serum phosphorous.
5) Treatment of rickets requires vitamin D, 50-150
micrograms once daily or 0.5-2.0 micrograms of
1,25-dihydroxycholecalciferol daily.
6) Secondary hyperparathyroidism occurs in
response to hypocalcemia which occurs in rickets. PTH
acts on the bone, kidney and intestine to have a net
effect of increasing serum calcium and decreasing
serum phosphorous. PTH acts to increase serum
calcium by releasing it directly from the bone. This
involves removal of bone and replacing it with osteoid
tissue, and in more advanced cases osteoid plus
fibrous tissue. Cystic degeneration later occurs within
this fibrous tissue; the cystic spaces being irregular at
first, but later becoming well defined. Conglomerations
of osteoclasts may eventually develop into large
tumours (osteoclastomata); so called "brown tumours."
Other radiographic findings are resorption of
subperiosteal bone, best seen along the margins of the
phalanges of the hands. In the skull there may be
gross trabeculations or a granular appearance resulting
from lytic skull lesions. Fractures can also occur.
About 10% of patients with hyperparathyroidism have
radiographic findings of rickets.
Refer to the forearm radiograph again.
Click on [Forearm]
As noted before, a right radial fracture is noted with
generalized severe demineralization, which can occur
solely due to rickets or secondary hyperparathyroidism.
Metaphyseal fraying and cuffing are noted, consistent
with rickets. Multiple lytic lucent lesions within the
diaphyses consistent with brown tumors are indicative
of secondary hyperparathyroidism.
References
1. Alagille D. Alagille syndrome today. Clinical
Invest Med 1996;19:325-330.
2. Hodson CJ. Metabolic and endocrine induced
bone disease. In: Shanks. Textbook of X-ray
Diagnosis, 4th Edition. Philadelphia, PA, W.B.
Saunders Co., 1971, pp. 685-695.
3. Krantz I, Piccoli D, Spinner N. Alagille syndrome.
J Med Genet 1997;34:152-157.
4. Mimouni F, Tsang RC. Parathyroid and vitamin
D-related disorders. In: Kaplan S. Clinical Pediatric
Endocrinology. Philadelphia, PA, W.B. Saunders Co.,
1990, pp. 427-452.
5. Pitt M. Rickets and osteomalacia are still around.
Radiologic Clinics of North America 1991;29:97-118.
6. Silverman F, Kuhn J. Metaholic abnormalities of
the skeleton. In: Caffey. Caffey's Pediatric Xray
Diagnosis, 9th Edition. St. Louis, MO, 1993, pp.
1746-1783.
7. Smith R. The pathophysiology and management
of rickets. Orthopedic Clinics of North America
1972;3:601-621.
These radiographs demonstrate epiphyseal and
metaphyseal flaring at the ends of the femur and tibia.
Lytic lesions are noted throughout the long bones.
These bony abnormalities are not primarily due to the
Alagille syndrome. What bony abnormality is present?
Teaching Points:
1) Alagille syndrome (arteriohepatic dysplasia) is
characterized by a paucity of intrahepatic bile
ducts. Clinical manifestations include chronic
cholestasis, characteristic facies, cardiovascular
abnormalities, vertebral arch defects and posterior
embryotoxin (an ocular accumulation of pigmentary
material). Cholestasis usually develops in the first few
months of life. Episodes of jaundice, are interspersed
with periods of anicteric remission. The characteristic
facies is observed in 95% of patients, consisting of a
prominent forehead, moderate hypertelorism with deep
set eyes, a small pointed chin, and a saddle or straight
nose. These features are usually not fully apparent
until 5-10 years of age.
The most common cardiovascular abnormality is
isolated and nonprogressive pulmonary stenosis of the
peripheral pulmonary vascular tree. The vertebral arch
defect seen is "butterfly-like" appearance of the dorsal
vertebrae. The accumulation of embryotoxin occurs in
more than 80% of patients with this syndrome.
Embryotoxin, a pigmentary material, accumulates in the
inner aspects of the cornea near its junction with the
iris. It is best observed with a slit lamp examination.
Other clinical manifestations include growth retardation,
renal abnormalities, mental retardation and voice
changes.
Chronic cholestasis can lead to malabsorption of fat
soluble vitamins due to lack of bile salts. Vitamin D
deficiency can result from this malabsorption as well
being due to a deficiency of 25-hydroxylation secondary
to destruction of liver parenchyma.
Diagnosis of Alagille syndrome is made by liver
biopsy and histological examination of the interlobular
bile ducts. This syndrome can be transmitted in an
autosomal dominant mode. Management includes a
high energy diet with adequate protein intake. Fat
soluble vitamins may need to be supplemented. There
is no way of predicting which patients (15%) will
progress to end stage liver disease and require
transplantation.
2) Our patient has severe demineralization and
pathologic fractures due to vitamin D deficiency
resulting in rickets. Rickets can be caused by dietary
deficiency, inadequate exposure to sunlight,
malabsorption and/or failure of metabolic activation of
vitamin D to the active form. Provitamin D3, is a
prohormone that eventually is converted to the active
form of vitamin D, 1,25-dihydroxyvitamin D3. This
active form increases intestinal calcium and
phosphorous absorption, mobilizes calcium and
phosphorous from bone to the bloodstream, and retains
calcium and phosphorous through its renal effect. This
renal effect moves calcium and phosphorous out of
older bone and also promotes the maturation and
mineralization of newly formed organic bone matrix.
In rickets, the main effect of vitamin D deficiency
results in a disorganization of the maturation and
calcification of the cartilage and its cells at the growing
ends of long bones. These abnormalities can be
correlated with radiographic findings. The widening and
lengthening of the physis represents the area of
disorganized mineralization in the zone of hypertrophy.
Widening and cupping of the metaphysis represents the
bulky mass of the hypertrophied zone placing abnormal
inward stress on the poorly mineralized metaphysis,
particularly on the more central areas.
3) The radiographic abnormalities seen in children
with rickets depend on the age of onset and duration
of illness.
a) Craniotabes: The head is particularly affected
during the first months of life. During this period, the
skull must accommodate the most rapidly growing
organ, the brain. The rapid accommodation by the skull
is associated with excess osteoid formation, particularly
at the central margins and outer table, while resorption
at the inner table continues. The thin calvarium is less
rigid and subject to supine postural influences, resulting
in posterior flattening. Continued accumulation of
osteoid in the frontal and parietal regions results in the
squared configuration known as craniotabes.
b) Long bone findings: During infancy and early
childhood, the long bones show the greatest deformity.
The metaphysis is widened, cupped and has a ragged
edge. There is a wide gap between the metaphysis and
the epiphysis corresponding to the area of disordered
mineralization. In mild cases the first radiologic sign is
a widening of the gap between the epiphysis and the
metaphysis. The characteristic bowing deformities of
the arms and legs are related to the sitting position
assumed by the child. Often, the child with severe
rickets will sit with his legs crossed. Bowing may also
result from asymmetric, musculotendinous forces that
displace the weakened growth plate. For example, the
Achilles tendon on the calcaneus displaces the distal
tibial growth plate resulting in the bowed tibia. The
shafts of long bones may also become less dense
caused by the loss of mineral content.
c) Rachitic rosary: Lumps develop at the
costochondral junctions, particularly those of the middle
ribs forming the characteristic rachitic rosary. The
costochondral junctions are the most active growth
plates and is the reason you see these changes here.
d) Harrison's groove: The distal end of the ribs are
weak and may be depressed by the negative
intrathoracic pressure developed during respiration with
a resultant semicoronal impression being found at the
costal attachment of the diaphragm, leading to the
formation of Harrison's groove.
e) Scoliosis: With increasing age, the effects of
weight bearing become prominent with scoliosis
frequently developing.
f) Looser's zones (pseudofractures): Rickets, later
in childhood, may have pseudofractures present.
Looser's zones are composed of focal accumulations of
osteoid, which is uncalcified bone matrix. They often
occur at sites where major arteries cross the bone and
have been thought to be secondary to the mechanical
stress of the pulsating vessel.
g) Fractures: Greenstick fractures of the cortex are
not uncommon.
4) Laboratory findings: In rickets, patients will have
an increased alkaline phosphatase >200, as in this
case. This is because of the active release of its stores
in bone. There are 3 stages of rickets. Stage I is the
early phase where serum calcium is low but serum
phosphorous is normal. In stage II, which occurs later,
serum calcium concentrations are restored to normal
ranges because of compensatory hyperparathyroidism,
but serum phosphorous levels are low. In stage III,
both serum calcium and phosphorous levels are low
and bone disease is florid because of the combined
effect of mineral deficiency and hyperparathyroidism.
This patient presented in stage II with a normal serum
calcium and low serum phosphorous.
5) Treatment of rickets requires vitamin D, 50-150
micrograms once daily or 0.5-2.0 micrograms of
1,25-dihydroxycholecalciferol daily.
6) Secondary hyperparathyroidism occurs in
response to hypocalcemia which occurs in rickets. PTH
acts on the bone, kidney and intestine to have a net
effect of increasing serum calcium and decreasing
serum phosphorous. PTH acts to increase serum
calcium by releasing it directly from the bone. This
involves removal of bone and replacing it with osteoid
tissue, and in more advanced cases osteoid plus
fibrous tissue. Cystic degeneration later occurs within
this fibrous tissue; the cystic spaces being irregular at
first, but later becoming well defined. Conglomerations
of osteoclasts may eventually develop into large
tumours (osteoclastomata); so called "brown tumours."
Other radiographic findings are resorption of
subperiosteal bone, best seen along the margins of the
phalanges of the hands. In the skull there may be
gross trabeculations or a granular appearance resulting
from lytic skull lesions. Fractures can also occur.
About 10% of patients with hyperparathyroidism have
radiographic findings of rickets.
Refer to the forearm radiograph again.
Click on [Forearm]
As noted before, a right radial fracture is noted with
generalized severe demineralization, which can occur
solely due to rickets or secondary hyperparathyroidism.
Metaphyseal fraying and cuffing are noted, consistent
with rickets. Multiple lytic lucent lesions within the
diaphyses consistent with brown tumors are indicative
of secondary hyperparathyroidism.
References
1. Alagille D. Alagille syndrome today. Clinical
Invest Med 1996;19:325-330.
2. Hodson CJ. Metabolic and endocrine induced
bone disease. In: Shanks. Textbook of X-ray
Diagnosis, 4th Edition. Philadelphia, PA, W.B.
Saunders Co., 1971, pp. 685-695.
3. Krantz I, Piccoli D, Spinner N. Alagille syndrome.
J Med Genet 1997;34:152-157.
4. Mimouni F, Tsang RC. Parathyroid and vitamin
D-related disorders. In: Kaplan S. Clinical Pediatric
Endocrinology. Philadelphia, PA, W.B. Saunders Co.,
1990, pp. 427-452.
5. Pitt M. Rickets and osteomalacia are still around.
Radiologic Clinics of North America 1991;29:97-118.
6. Silverman F, Kuhn J. Metaholic abnormalities of
the skeleton. In: Caffey. Caffey's Pediatric Xray
Diagnosis, 9th Edition. St. Louis, MO, 1993, pp.
1746-1783.
7. Smith R. The pathophysiology and management
of rickets. Orthopedic Clinics of North America
1972;3:601-621.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 The radiograph demonstrates a healing right radial
midshaft fracture. Also noted are multiple lytic lesions
with cortical scalloping along the metaphysis and
diaphysis of the forearm bones with generalized severe
demineralization. A long bone survey is obtained.
View his lower extremity radiographs.
View femur radiographs.
The radiograph demonstrates a healing right radial
midshaft fracture. Also noted are multiple lytic lesions
with cortical scalloping along the metaphysis and
diaphysis of the forearm bones with generalized severe
demineralization. A long bone survey is obtained.
View his lower extremity radiographs.
View femur radiographs.
 View tibia radiographs.
View tibia radiographs.
 These radiographs demonstrate epiphyseal and
metaphyseal flaring at the ends of the femur and tibia.
Lytic lesions are noted throughout the long bones.
These bony abnormalities are not primarily due to the
Alagille syndrome. What bony abnormality is present?
Teaching Points:
1) Alagille syndrome (arteriohepatic dysplasia) is
characterized by a paucity of intrahepatic bile
ducts. Clinical manifestations include chronic
cholestasis, characteristic facies, cardiovascular
abnormalities, vertebral arch defects and posterior
embryotoxin (an ocular accumulation of pigmentary
material). Cholestasis usually develops in the first few
months of life. Episodes of jaundice, are interspersed
with periods of anicteric remission. The characteristic
facies is observed in 95% of patients, consisting of a
prominent forehead, moderate hypertelorism with deep
set eyes, a small pointed chin, and a saddle or straight
nose. These features are usually not fully apparent
until 5-10 years of age.
The most common cardiovascular abnormality is
isolated and nonprogressive pulmonary stenosis of the
peripheral pulmonary vascular tree. The vertebral arch
defect seen is "butterfly-like" appearance of the dorsal
vertebrae. The accumulation of embryotoxin occurs in
more than 80% of patients with this syndrome.
Embryotoxin, a pigmentary material, accumulates in the
inner aspects of the cornea near its junction with the
iris. It is best observed with a slit lamp examination.
Other clinical manifestations include growth retardation,
renal abnormalities, mental retardation and voice
changes.
Chronic cholestasis can lead to malabsorption of fat
soluble vitamins due to lack of bile salts. Vitamin D
deficiency can result from this malabsorption as well
being due to a deficiency of 25-hydroxylation secondary
to destruction of liver parenchyma.
Diagnosis of Alagille syndrome is made by liver
biopsy and histological examination of the interlobular
bile ducts. This syndrome can be transmitted in an
autosomal dominant mode. Management includes a
high energy diet with adequate protein intake. Fat
soluble vitamins may need to be supplemented. There
is no way of predicting which patients (15%) will
progress to end stage liver disease and require
transplantation.
2) Our patient has severe demineralization and
pathologic fractures due to vitamin D deficiency
resulting in rickets. Rickets can be caused by dietary
deficiency, inadequate exposure to sunlight,
malabsorption and/or failure of metabolic activation of
vitamin D to the active form. Provitamin D3, is a
prohormone that eventually is converted to the active
form of vitamin D, 1,25-dihydroxyvitamin D3. This
active form increases intestinal calcium and
phosphorous absorption, mobilizes calcium and
phosphorous from bone to the bloodstream, and retains
calcium and phosphorous through its renal effect. This
renal effect moves calcium and phosphorous out of
older bone and also promotes the maturation and
mineralization of newly formed organic bone matrix.
In rickets, the main effect of vitamin D deficiency
results in a disorganization of the maturation and
calcification of the cartilage and its cells at the growing
ends of long bones. These abnormalities can be
correlated with radiographic findings. The widening and
lengthening of the physis represents the area of
disorganized mineralization in the zone of hypertrophy.
Widening and cupping of the metaphysis represents the
bulky mass of the hypertrophied zone placing abnormal
inward stress on the poorly mineralized metaphysis,
particularly on the more central areas.
3) The radiographic abnormalities seen in children
with rickets depend on the age of onset and duration
of illness.
a) Craniotabes: The head is particularly affected
during the first months of life. During this period, the
skull must accommodate the most rapidly growing
organ, the brain. The rapid accommodation by the skull
is associated with excess osteoid formation, particularly
at the central margins and outer table, while resorption
at the inner table continues. The thin calvarium is less
rigid and subject to supine postural influences, resulting
in posterior flattening. Continued accumulation of
osteoid in the frontal and parietal regions results in the
squared configuration known as craniotabes.
b) Long bone findings: During infancy and early
childhood, the long bones show the greatest deformity.
The metaphysis is widened, cupped and has a ragged
edge. There is a wide gap between the metaphysis and
the epiphysis corresponding to the area of disordered
mineralization. In mild cases the first radiologic sign is
a widening of the gap between the epiphysis and the
metaphysis. The characteristic bowing deformities of
the arms and legs are related to the sitting position
assumed by the child. Often, the child with severe
rickets will sit with his legs crossed. Bowing may also
result from asymmetric, musculotendinous forces that
displace the weakened growth plate. For example, the
Achilles tendon on the calcaneus displaces the distal
tibial growth plate resulting in the bowed tibia. The
shafts of long bones may also become less dense
caused by the loss of mineral content.
c) Rachitic rosary: Lumps develop at the
costochondral junctions, particularly those of the middle
ribs forming the characteristic rachitic rosary. The
costochondral junctions are the most active growth
plates and is the reason you see these changes here.
d) Harrison's groove: The distal end of the ribs are
weak and may be depressed by the negative
intrathoracic pressure developed during respiration with
a resultant semicoronal impression being found at the
costal attachment of the diaphragm, leading to the
formation of Harrison's groove.
e) Scoliosis: With increasing age, the effects of
weight bearing become prominent with scoliosis
frequently developing.
f) Looser's zones (pseudofractures): Rickets, later
in childhood, may have pseudofractures present.
Looser's zones are composed of focal accumulations of
osteoid, which is uncalcified bone matrix. They often
occur at sites where major arteries cross the bone and
have been thought to be secondary to the mechanical
stress of the pulsating vessel.
g) Fractures: Greenstick fractures of the cortex are
not uncommon.
4) Laboratory findings: In rickets, patients will have
an increased alkaline phosphatase >200, as in this
case. This is because of the active release of its stores
in bone. There are 3 stages of rickets. Stage I is the
early phase where serum calcium is low but serum
phosphorous is normal. In stage II, which occurs later,
serum calcium concentrations are restored to normal
ranges because of compensatory hyperparathyroidism,
but serum phosphorous levels are low. In stage III,
both serum calcium and phosphorous levels are low
and bone disease is florid because of the combined
effect of mineral deficiency and hyperparathyroidism.
This patient presented in stage II with a normal serum
calcium and low serum phosphorous.
5) Treatment of rickets requires vitamin D, 50-150
micrograms once daily or 0.5-2.0 micrograms of
1,25-dihydroxycholecalciferol daily.
6) Secondary hyperparathyroidism occurs in
response to hypocalcemia which occurs in rickets. PTH
acts on the bone, kidney and intestine to have a net
effect of increasing serum calcium and decreasing
serum phosphorous. PTH acts to increase serum
calcium by releasing it directly from the bone. This
involves removal of bone and replacing it with osteoid
tissue, and in more advanced cases osteoid plus
fibrous tissue. Cystic degeneration later occurs within
this fibrous tissue; the cystic spaces being irregular at
first, but later becoming well defined. Conglomerations
of osteoclasts may eventually develop into large
tumours (osteoclastomata); so called "brown tumours."
Other radiographic findings are resorption of
subperiosteal bone, best seen along the margins of the
phalanges of the hands. In the skull there may be
gross trabeculations or a granular appearance resulting
from lytic skull lesions. Fractures can also occur.
About 10% of patients with hyperparathyroidism have
radiographic findings of rickets.
Refer to the forearm radiograph again.
Click on [Forearm]
As noted before, a right radial fracture is noted with
generalized severe demineralization, which can occur
solely due to rickets or secondary hyperparathyroidism.
Metaphyseal fraying and cuffing are noted, consistent
with rickets. Multiple lytic lucent lesions within the
diaphyses consistent with brown tumors are indicative
of secondary hyperparathyroidism.
References
1. Alagille D. Alagille syndrome today. Clinical
Invest Med 1996;19:325-330.
2. Hodson CJ. Metabolic and endocrine induced
bone disease. In: Shanks. Textbook of X-ray
Diagnosis, 4th Edition. Philadelphia, PA, W.B.
Saunders Co., 1971, pp. 685-695.
3. Krantz I, Piccoli D, Spinner N. Alagille syndrome.
J Med Genet 1997;34:152-157.
4. Mimouni F, Tsang RC. Parathyroid and vitamin
D-related disorders. In: Kaplan S. Clinical Pediatric
Endocrinology. Philadelphia, PA, W.B. Saunders Co.,
1990, pp. 427-452.
5. Pitt M. Rickets and osteomalacia are still around.
Radiologic Clinics of North America 1991;29:97-118.
6. Silverman F, Kuhn J. Metaholic abnormalities of
the skeleton. In: Caffey. Caffey's Pediatric Xray
Diagnosis, 9th Edition. St. Louis, MO, 1993, pp.
1746-1783.
7. Smith R. The pathophysiology and management
of rickets. Orthopedic Clinics of North America
1972;3:601-621.
These radiographs demonstrate epiphyseal and
metaphyseal flaring at the ends of the femur and tibia.
Lytic lesions are noted throughout the long bones.
These bony abnormalities are not primarily due to the
Alagille syndrome. What bony abnormality is present?
Teaching Points:
1) Alagille syndrome (arteriohepatic dysplasia) is
characterized by a paucity of intrahepatic bile
ducts. Clinical manifestations include chronic
cholestasis, characteristic facies, cardiovascular
abnormalities, vertebral arch defects and posterior
embryotoxin (an ocular accumulation of pigmentary
material). Cholestasis usually develops in the first few
months of life. Episodes of jaundice, are interspersed
with periods of anicteric remission. The characteristic
facies is observed in 95% of patients, consisting of a
prominent forehead, moderate hypertelorism with deep
set eyes, a small pointed chin, and a saddle or straight
nose. These features are usually not fully apparent
until 5-10 years of age.
The most common cardiovascular abnormality is
isolated and nonprogressive pulmonary stenosis of the
peripheral pulmonary vascular tree. The vertebral arch
defect seen is "butterfly-like" appearance of the dorsal
vertebrae. The accumulation of embryotoxin occurs in
more than 80% of patients with this syndrome.
Embryotoxin, a pigmentary material, accumulates in the
inner aspects of the cornea near its junction with the
iris. It is best observed with a slit lamp examination.
Other clinical manifestations include growth retardation,
renal abnormalities, mental retardation and voice
changes.
Chronic cholestasis can lead to malabsorption of fat
soluble vitamins due to lack of bile salts. Vitamin D
deficiency can result from this malabsorption as well
being due to a deficiency of 25-hydroxylation secondary
to destruction of liver parenchyma.
Diagnosis of Alagille syndrome is made by liver
biopsy and histological examination of the interlobular
bile ducts. This syndrome can be transmitted in an
autosomal dominant mode. Management includes a
high energy diet with adequate protein intake. Fat
soluble vitamins may need to be supplemented. There
is no way of predicting which patients (15%) will
progress to end stage liver disease and require
transplantation.
2) Our patient has severe demineralization and
pathologic fractures due to vitamin D deficiency
resulting in rickets. Rickets can be caused by dietary
deficiency, inadequate exposure to sunlight,
malabsorption and/or failure of metabolic activation of
vitamin D to the active form. Provitamin D3, is a
prohormone that eventually is converted to the active
form of vitamin D, 1,25-dihydroxyvitamin D3. This
active form increases intestinal calcium and
phosphorous absorption, mobilizes calcium and
phosphorous from bone to the bloodstream, and retains
calcium and phosphorous through its renal effect. This
renal effect moves calcium and phosphorous out of
older bone and also promotes the maturation and
mineralization of newly formed organic bone matrix.
In rickets, the main effect of vitamin D deficiency
results in a disorganization of the maturation and
calcification of the cartilage and its cells at the growing
ends of long bones. These abnormalities can be
correlated with radiographic findings. The widening and
lengthening of the physis represents the area of
disorganized mineralization in the zone of hypertrophy.
Widening and cupping of the metaphysis represents the
bulky mass of the hypertrophied zone placing abnormal
inward stress on the poorly mineralized metaphysis,
particularly on the more central areas.
3) The radiographic abnormalities seen in children
with rickets depend on the age of onset and duration
of illness.
a) Craniotabes: The head is particularly affected
during the first months of life. During this period, the
skull must accommodate the most rapidly growing
organ, the brain. The rapid accommodation by the skull
is associated with excess osteoid formation, particularly
at the central margins and outer table, while resorption
at the inner table continues. The thin calvarium is less
rigid and subject to supine postural influences, resulting
in posterior flattening. Continued accumulation of
osteoid in the frontal and parietal regions results in the
squared configuration known as craniotabes.
b) Long bone findings: During infancy and early
childhood, the long bones show the greatest deformity.
The metaphysis is widened, cupped and has a ragged
edge. There is a wide gap between the metaphysis and
the epiphysis corresponding to the area of disordered
mineralization. In mild cases the first radiologic sign is
a widening of the gap between the epiphysis and the
metaphysis. The characteristic bowing deformities of
the arms and legs are related to the sitting position
assumed by the child. Often, the child with severe
rickets will sit with his legs crossed. Bowing may also
result from asymmetric, musculotendinous forces that
displace the weakened growth plate. For example, the
Achilles tendon on the calcaneus displaces the distal
tibial growth plate resulting in the bowed tibia. The
shafts of long bones may also become less dense
caused by the loss of mineral content.
c) Rachitic rosary: Lumps develop at the
costochondral junctions, particularly those of the middle
ribs forming the characteristic rachitic rosary. The
costochondral junctions are the most active growth
plates and is the reason you see these changes here.
d) Harrison's groove: The distal end of the ribs are
weak and may be depressed by the negative
intrathoracic pressure developed during respiration with
a resultant semicoronal impression being found at the
costal attachment of the diaphragm, leading to the
formation of Harrison's groove.
e) Scoliosis: With increasing age, the effects of
weight bearing become prominent with scoliosis
frequently developing.
f) Looser's zones (pseudofractures): Rickets, later
in childhood, may have pseudofractures present.
Looser's zones are composed of focal accumulations of
osteoid, which is uncalcified bone matrix. They often
occur at sites where major arteries cross the bone and
have been thought to be secondary to the mechanical
stress of the pulsating vessel.
g) Fractures: Greenstick fractures of the cortex are
not uncommon.
4) Laboratory findings: In rickets, patients will have
an increased alkaline phosphatase >200, as in this
case. This is because of the active release of its stores
in bone. There are 3 stages of rickets. Stage I is the
early phase where serum calcium is low but serum
phosphorous is normal. In stage II, which occurs later,
serum calcium concentrations are restored to normal
ranges because of compensatory hyperparathyroidism,
but serum phosphorous levels are low. In stage III,
both serum calcium and phosphorous levels are low
and bone disease is florid because of the combined
effect of mineral deficiency and hyperparathyroidism.
This patient presented in stage II with a normal serum
calcium and low serum phosphorous.
5) Treatment of rickets requires vitamin D, 50-150
micrograms once daily or 0.5-2.0 micrograms of
1,25-dihydroxycholecalciferol daily.
6) Secondary hyperparathyroidism occurs in
response to hypocalcemia which occurs in rickets. PTH
acts on the bone, kidney and intestine to have a net
effect of increasing serum calcium and decreasing
serum phosphorous. PTH acts to increase serum
calcium by releasing it directly from the bone. This
involves removal of bone and replacing it with osteoid
tissue, and in more advanced cases osteoid plus
fibrous tissue. Cystic degeneration later occurs within
this fibrous tissue; the cystic spaces being irregular at
first, but later becoming well defined. Conglomerations
of osteoclasts may eventually develop into large
tumours (osteoclastomata); so called "brown tumours."
Other radiographic findings are resorption of
subperiosteal bone, best seen along the margins of the
phalanges of the hands. In the skull there may be
gross trabeculations or a granular appearance resulting
from lytic skull lesions. Fractures can also occur.
About 10% of patients with hyperparathyroidism have
radiographic findings of rickets.
Refer to the forearm radiograph again.
Click on [Forearm]
As noted before, a right radial fracture is noted with
generalized severe demineralization, which can occur
solely due to rickets or secondary hyperparathyroidism.
Metaphyseal fraying and cuffing are noted, consistent
with rickets. Multiple lytic lucent lesions within the
diaphyses consistent with brown tumors are indicative
of secondary hyperparathyroidism.
References
1. Alagille D. Alagille syndrome today. Clinical
Invest Med 1996;19:325-330.
2. Hodson CJ. Metabolic and endocrine induced
bone disease. In: Shanks. Textbook of X-ray
Diagnosis, 4th Edition. Philadelphia, PA, W.B.
Saunders Co., 1971, pp. 685-695.
3. Krantz I, Piccoli D, Spinner N. Alagille syndrome.
J Med Genet 1997;34:152-157.
4. Mimouni F, Tsang RC. Parathyroid and vitamin
D-related disorders. In: Kaplan S. Clinical Pediatric
Endocrinology. Philadelphia, PA, W.B. Saunders Co.,
1990, pp. 427-452.
5. Pitt M. Rickets and osteomalacia are still around.
Radiologic Clinics of North America 1991;29:97-118.
6. Silverman F, Kuhn J. Metaholic abnormalities of
the skeleton. In: Caffey. Caffey's Pediatric Xray
Diagnosis, 9th Edition. St. Louis, MO, 1993, pp.
1746-1783.
7. Smith R. The pathophysiology and management
of rickets. Orthopedic Clinics of North America
1972;3:601-621.