Cervical Spine Radiographs
Radiology Cases in Pediatric Emergency Medicine
Volume 5, Case 2
Tai-Chuen Lin, Medical Student
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
Introductory Notes
Most spinal cord injuries are attributed to trauma.
Absence of radiographic findings does not exclude a
spinal cord injury. A substantial portion of spinal cord
injuries in children (25% to 50%) have no radiographic
abnormalities--SCIWORA (spinal cord injury without
radiographic abnormalities). Some patients with
cervical spine injury may also have thoracolumbar
lesions. In the younger child, injuries to the cervical
spine often involve the upper three vertebrae.
Pediatric Considerations
Pediatric anatomy differs from the adult in several
important ways, particularly in the ossification pattern of
the cervicocranium (occiput-atlas-axis) and the normal
laxity of the developing soft tissue structures of the
cervicocranium. These differences can lead to false
positive interpretation as fractures, subluxations, and/or
tumors etc. (Refer to Case 5 of Volume 1, Cervical
Spine Malalignment - True or Pseudo Subluxation?,
and Case 1 of Volume 5, Fever With Neck Stiffness . . .
Rule Out Meningitis).
Clinical Aspects
The assessment of cervical spine injuries must first
be a clinical evaluation. Clinical and radiographic data
should be interpreted together to yield the most
accurate assessment.
Diagnostic strategies depend on whether the patient
is conscious and can freely move his or her neck.
Unconscious or poorly conscious patients should be
examined radiographically while maintaining cervical
spine immobilization since history and examination will
be unreliable.
A conscious patient with a significant cervical spine
injury will complain of pain. A significant cervical spine
injury is not likely to be present in a patient without neck
pain who is alert, not intoxicated, and lacks other painful
injuries (that may distract neck pain). Normal cervical
range of motion is consistent with the absence of a
cervical spine injury and such patients generally do not
need any radiographs.
Anatomy
In order to properly evaluate the radiographic
images of the cervical spine, an understanding of the
cervical spine anatomy is necessary to appreciate the
structural organization that lends to spinal stability. The
vertebrae are bony building blocks connected by
ligamentous and muscular structures. This resulting
stable skeleton provides the scaffold for the soft tissue
structures that communicate between the head and the
thorax, the spinal cord being one of the most delicate
and important.
The cervical spine is made up of seven sequentially
numbered cervical vertebrae, C1 through C7.
Superiorly, C1 is connected to the occiput of the
cranium. Inferiorly, C7 is connected to the first thoracic
vertebrae, T1. The upper portion of the cervical spine,
C1 and C2, together with the occiput is also referred to
as the cervicocranium. All vertebrae share many
common features. These will be reviewed along with
features unique to the cervical vertebrae. C1 and C2
are atypical cervical vertebrae and will be treated
separately.
Vertebral Body
The anterior and most easily identifiable structure of
a vertebra is the vertebral body, also known as the
centrum. The body is the largest and appropriately the
main weight-bearing structure of a vertebra. The back
of the body also forms the anterior border of the spinal
canal.
View C4.
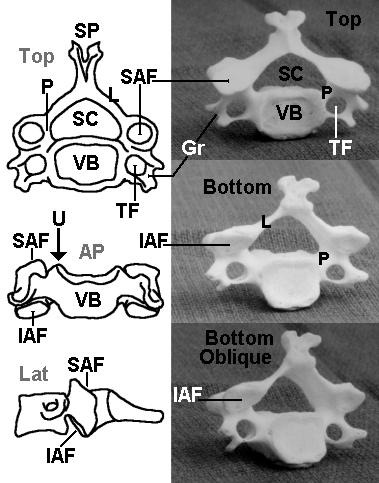
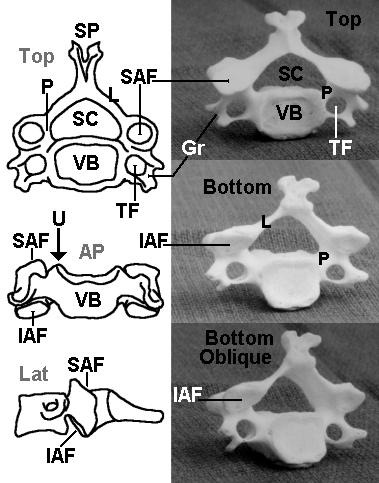
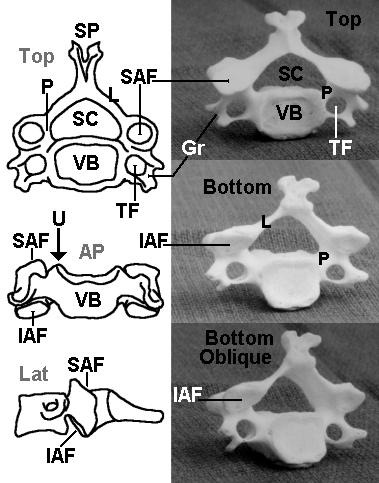
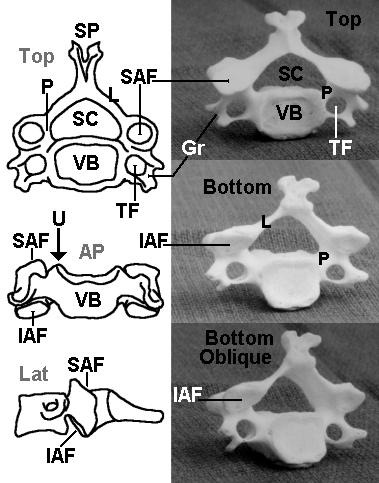
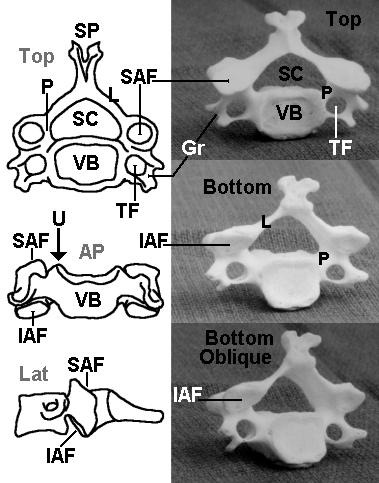
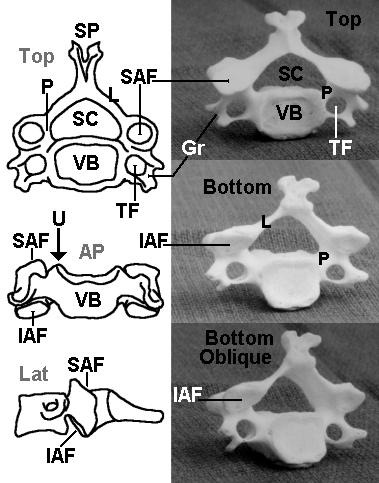 The three line diagrams on the left from top to
bottom include an axial view, viewed from the top (Top),
an anterior view (AP), and a lateral view (Lat). The
three photographs of C4 on the right from top to bottom
include a view from the top (Top), a view from the
bottom (Bottom), and an oblique view from the bottom
(Bottom oblique).
Identify the following structures on these diagrams
and photos:
SP - spinous process
L - lamina (forms roof of the neural arch)
P - pedicle (forms supports of the neural arch)
SC - spinal canal
VB - vertebral body
SAF - superior articular facet
IAF - inferior articular facet
TF - transverse foramen
Gr - groove for spinal nerve (transverse process)
U - uncinate process
The neural arch is formed by the laminae, the base
of the spinous process and the pedicles. The pedicles
are very short in the cervical spine. The facet joints are
formed by the inferior and superior facets such that the
C4-C5 facet joint is formed by the inferior articular facet
of C4 and the superior articular facet of C5.
On a lateral film, the body is a rhomboid with the
posterior portion slightly taller than the anterior portion.
View lateral C-spine view.
The three line diagrams on the left from top to
bottom include an axial view, viewed from the top (Top),
an anterior view (AP), and a lateral view (Lat). The
three photographs of C4 on the right from top to bottom
include a view from the top (Top), a view from the
bottom (Bottom), and an oblique view from the bottom
(Bottom oblique).
Identify the following structures on these diagrams
and photos:
SP - spinous process
L - lamina (forms roof of the neural arch)
P - pedicle (forms supports of the neural arch)
SC - spinal canal
VB - vertebral body
SAF - superior articular facet
IAF - inferior articular facet
TF - transverse foramen
Gr - groove for spinal nerve (transverse process)
U - uncinate process
The neural arch is formed by the laminae, the base
of the spinous process and the pedicles. The pedicles
are very short in the cervical spine. The facet joints are
formed by the inferior and superior facets such that the
C4-C5 facet joint is formed by the inferior articular facet
of C4 and the superior articular facet of C5.
On a lateral film, the body is a rhomboid with the
posterior portion slightly taller than the anterior portion.
View lateral C-spine view.
 The lateral view of a very young child is shown on
the left compared to the lateral view of a teenager on
the right. Alignment is assessed by the integrity of lines
drawn along: 1) the anterior borders of the vertebral
bodies, 2) the posterior borders of the vertebral bodies
and 3) the anterior borders of the vertebral arch's apex
(spinolaminal line). The facet joints should be clearly
visible.
View identifying landmarks.
The lateral view of a very young child is shown on
the left compared to the lateral view of a teenager on
the right. Alignment is assessed by the integrity of lines
drawn along: 1) the anterior borders of the vertebral
bodies, 2) the posterior borders of the vertebral bodies
and 3) the anterior borders of the vertebral arch's apex
(spinolaminal line). The facet joints should be clearly
visible.
View identifying landmarks.
 The contour lines of alignment are shown. Identify
the following areas on the radiographs:
F - facet joint
SP - spinous process
L - lamina
Od - odontoid
On an AP view, the lateral superior edges of the
body form bilateral ridges, called the uncinate
processes (U).
View AP C-spine view.
The contour lines of alignment are shown. Identify
the following areas on the radiographs:
F - facet joint
SP - spinous process
L - lamina
Od - odontoid
On an AP view, the lateral superior edges of the
body form bilateral ridges, called the uncinate
processes (U).
View AP C-spine view.
 A posterior view of the cervical spine is shown on
the left. An anterior view is shown in the center.
Axial compression can result in compression
fractures which can lead to decreased vertebral body
height or a burst fracture that fragments the vertebral
body. A strong lateral force can cause a shearing
action and create fractures of an uncinate process.
Hyperflexion and hyperextension may also result in
teardrop fractures of the anterior superior or inferior
corner of the body.
Between the vertebral bodies are the intervertebral
disks. These function as shock absorbers. As in the
lumbar region, rupture of the annulus can lead to
encroachment into the spinal canal. The vertebral body
also serves as the attachment site of the anterior and
posterior longitudinal ligaments. Tears in these
ligamentous structures can result from displacement or
extensive fractures of the vertebral body. Without
these ligamentous connections, the vertebral column is
unstable.
Neural Arch
Posterior to the vertebral body is the neural arch
(vertebral arch covering the spinal canal). The neural
arch refers to all the structures dorsal to the body. The
arch serves to protect the spinal cord, provide
attachment sites for ligaments and muscles, and forms
synovial joints that facilitate movement of the vertebral
column. The major structures that make up the arch
include: 1) the pedicles, 2) the laminae, 3) the spinous
process, 4) the articular processes and facets, and 5)
the transverse processes.
View C4.
A posterior view of the cervical spine is shown on
the left. An anterior view is shown in the center.
Axial compression can result in compression
fractures which can lead to decreased vertebral body
height or a burst fracture that fragments the vertebral
body. A strong lateral force can cause a shearing
action and create fractures of an uncinate process.
Hyperflexion and hyperextension may also result in
teardrop fractures of the anterior superior or inferior
corner of the body.
Between the vertebral bodies are the intervertebral
disks. These function as shock absorbers. As in the
lumbar region, rupture of the annulus can lead to
encroachment into the spinal canal. The vertebral body
also serves as the attachment site of the anterior and
posterior longitudinal ligaments. Tears in these
ligamentous structures can result from displacement or
extensive fractures of the vertebral body. Without
these ligamentous connections, the vertebral column is
unstable.
Neural Arch
Posterior to the vertebral body is the neural arch
(vertebral arch covering the spinal canal). The neural
arch refers to all the structures dorsal to the body. The
arch serves to protect the spinal cord, provide
attachment sites for ligaments and muscles, and forms
synovial joints that facilitate movement of the vertebral
column. The major structures that make up the arch
include: 1) the pedicles, 2) the laminae, 3) the spinous
process, 4) the articular processes and facets, and 5)
the transverse processes.
View C4.
 Pedicles
The pedicles ("little feet") form the supports of the
neural arch as it is attached to the vertebral body. In
the cervical spine, the pedicles are short. They project
posteriorly (dorsally) from the body and form the lateral
borders of the spinal canal. Superior and slightly larger
inferior vertebral notches above and below the pedicles
form intervertebral foramina in the articulated vertebral
column. Through these foramina pass the cervical
spinal nerves.
View lateral.
Pedicles
The pedicles ("little feet") form the supports of the
neural arch as it is attached to the vertebral body. In
the cervical spine, the pedicles are short. They project
posteriorly (dorsally) from the body and form the lateral
borders of the spinal canal. Superior and slightly larger
inferior vertebral notches above and below the pedicles
form intervertebral foramina in the articulated vertebral
column. Through these foramina pass the cervical
spinal nerves.
View lateral.
 On a lateral film, the pedicles appear as small
connections between the body and the articular
processes (see below). On the AP view, the pedicles
appear as small doughnut densities on the lateral upper
portion of the vertebral body, just below the uncinate
processes. Fractures in this region can disrupt the
spinal nerves or the spinal cord itself.
View AP.
On a lateral film, the pedicles appear as small
connections between the body and the articular
processes (see below). On the AP view, the pedicles
appear as small doughnut densities on the lateral upper
portion of the vertebral body, just below the uncinate
processes. Fractures in this region can disrupt the
spinal nerves or the spinal cord itself.
View AP.
 Laminae
The laminae (meaning "layers") form a roof over
the neural arch, supported by the pedicles. In addition
to the obvious protective function, the laminae also
serve as the site of attachment for the ligamentum
flavum. Because the laminae are thinner in the C-spine
compared to other vertebrae, their relative radiolucency
appears as an apparent gap between the posterior
cortex of the articular facets and the anterior cortex of
the spinous process (posterior aspect of the neural
arch) on the lateral view. In general, the laminae (L)
are not easily appreciable on an AP view.
View lateral.
Laminae
The laminae (meaning "layers") form a roof over
the neural arch, supported by the pedicles. In addition
to the obvious protective function, the laminae also
serve as the site of attachment for the ligamentum
flavum. Because the laminae are thinner in the C-spine
compared to other vertebrae, their relative radiolucency
appears as an apparent gap between the posterior
cortex of the articular facets and the anterior cortex of
the spinous process (posterior aspect of the neural
arch) on the lateral view. In general, the laminae (L)
are not easily appreciable on an AP view.
View lateral.
 Spinous Process
The spinous process projects dorsoinferiorly from
the point of union of the laminae. Unique to the typical
cervical vertebrae, the spinous processes of C3 through
C6 are typically bifid at the tips. The spine of C7 is an
easily visible surface landmark called the vertebra
prominens. The spinous processes are the site of
attachment for a number of ligamentous and tendinous
structures. The major ligaments associated with the
spine include the interspinous and supraspinous
ligaments as well as the ligamentum nuchae. A number
of intrinsic muscles of the spine as well as large back
muscles such as the trapezius, the levator scapularis,
and the rhomboids are attached to the cervical spinous
processes. Excessive load on these muscles may
result in avulsion of the spinous processes of C6 and
C7, commonly known as the clay shoveller's fracture.
This fracture is more commonly found in adults.
View lateral.
Spinous Process
The spinous process projects dorsoinferiorly from
the point of union of the laminae. Unique to the typical
cervical vertebrae, the spinous processes of C3 through
C6 are typically bifid at the tips. The spine of C7 is an
easily visible surface landmark called the vertebra
prominens. The spinous processes are the site of
attachment for a number of ligamentous and tendinous
structures. The major ligaments associated with the
spine include the interspinous and supraspinous
ligaments as well as the ligamentum nuchae. A number
of intrinsic muscles of the spine as well as large back
muscles such as the trapezius, the levator scapularis,
and the rhomboids are attached to the cervical spinous
processes. Excessive load on these muscles may
result in avulsion of the spinous processes of C6 and
C7, commonly known as the clay shoveller's fracture.
This fracture is more commonly found in adults.
View lateral.
 On a lateral view, the spinous processes appear as
triangular extensions. The anterior border with the
laminae (spinolaminal line) is an easily visible feature
marking the posterior border of the vertebral canal
(spinal canal). On an AP view, the spinous processes
appear as a midline density superimposed on the
vertebral body. The bifid nature of some of the cervical
spines can be easily appreciated in this view.
View AP.
On a lateral view, the spinous processes appear as
triangular extensions. The anterior border with the
laminae (spinolaminal line) is an easily visible feature
marking the posterior border of the vertebral canal
(spinal canal). On an AP view, the spinous processes
appear as a midline density superimposed on the
vertebral body. The bifid nature of some of the cervical
spines can be easily appreciated in this view.
View AP.
 Articular Processes and Articular Facets
The articular processes are cylindrical structures at
the junction of the pedicles and the laminae. Like the
pedicles, articular processes also delimit the lateral
margins of the spinal canal. The articular facets, the
oblique elliptical ends of the cylinders, are higher
anteriorly and lower posteriorly.
View articular facets of C4.
Articular Processes and Articular Facets
The articular processes are cylindrical structures at
the junction of the pedicles and the laminae. Like the
pedicles, articular processes also delimit the lateral
margins of the spinal canal. The articular facets, the
oblique elliptical ends of the cylinders, are higher
anteriorly and lower posteriorly.
View articular facets of C4.
 Capsular articular ligaments join adjacent inferior
and superior articular facets of successive vertebrae to
form synovial joints. Strong rotary forces can stretch or
tear these ligaments resulting in unilateral or bilateral
dislocated facets.
View lateral.
Capsular articular ligaments join adjacent inferior
and superior articular facets of successive vertebrae to
form synovial joints. Strong rotary forces can stretch or
tear these ligaments resulting in unilateral or bilateral
dislocated facets.
View lateral.
 On a lateral view, the articular processes are
rhomboidal in shape and superimposed upon one
another. Unlike the vertebral body which slopes
downward anteriorly, the articular processes slope
sharply downward posteriorly. They appear
superimposed on the spinal canal.
View oblique view.
On a lateral view, the articular processes are
rhomboidal in shape and superimposed upon one
another. Unlike the vertebral body which slopes
downward anteriorly, the articular processes slope
sharply downward posteriorly. They appear
superimposed on the spinal canal.
View oblique view.
 The skeletal model on the left shows variability in
the intervertebral disk spacing due to poor positioning of
the model bones during photography. This oblique view
shows the intervertebral foramina formed by the inferior
notch of the pedicle of the vertebrae above and the
superior notch of the pedicle of the vertebrae below.
Transverse Processes
The transverse processes project outward
anteroinferiorly from the pedicles like half-cylindrical
scoops.
View C4.
The skeletal model on the left shows variability in
the intervertebral disk spacing due to poor positioning of
the model bones during photography. This oblique view
shows the intervertebral foramina formed by the inferior
notch of the pedicle of the vertebrae above and the
superior notch of the pedicle of the vertebrae below.
Transverse Processes
The transverse processes project outward
anteroinferiorly from the pedicles like half-cylindrical
scoops.
View C4.
 Along the grooved portion of the transverse
process pass the ventral rami of the cervical nerves.
The dorsal rami pass more posteriorly. In the middle
of the transverse process is a foramen for the vertebral
artery as it courses upward toward the foramen
magnum. Lesions in this region can damage the
nerves of cervical and brachial plexi as well as
compromise the arterial supply of the posterior brain.
The Cervicocranium
The articulations between the occiput, the atlas
(C1), and the axis (C2) are highly specialized to allow
the extensive range of motion of the head upon the
neck. As such, C1 and C2 differ sufficiently from the
typical vertebrae that they deserve special mention.
View odontoid view.
Along the grooved portion of the transverse
process pass the ventral rami of the cervical nerves.
The dorsal rami pass more posteriorly. In the middle
of the transverse process is a foramen for the vertebral
artery as it courses upward toward the foramen
magnum. Lesions in this region can damage the
nerves of cervical and brachial plexi as well as
compromise the arterial supply of the posterior brain.
The Cervicocranium
The articulations between the occiput, the atlas
(C1), and the axis (C2) are highly specialized to allow
the extensive range of motion of the head upon the
neck. As such, C1 and C2 differ sufficiently from the
typical vertebrae that they deserve special mention.
View odontoid view.
 The atlas (C1) articulates superiorly with the
occipital bone. The occipital bone forms the base of the
cranium, and articulation with the cervical spine is via
the pair of large convex occipital condyles situated on
either side of the anterior half of the foramen magnum.
The brain stem becomes the spinal cord as it leaves the
cranium through the foramen magnum. Anterior to the
foramen magnum is an upward incline to the dorsum
sellae called the clivus. The posterior aspect of the
foramen magnum is in-line with the posterior arch of C1
and C2 (the spinolaminar line).
Lacking a body, the atlas is essentially a ring with
prominent articular processes that are appropriately
called lateral masses. The lateral masses divide the
ring into a smaller anterior and a larger posterior arch.
View C1-C2 cross section CT scan.
The atlas (C1) articulates superiorly with the
occipital bone. The occipital bone forms the base of the
cranium, and articulation with the cervical spine is via
the pair of large convex occipital condyles situated on
either side of the anterior half of the foramen magnum.
The brain stem becomes the spinal cord as it leaves the
cranium through the foramen magnum. Anterior to the
foramen magnum is an upward incline to the dorsum
sellae called the clivus. The posterior aspect of the
foramen magnum is in-line with the posterior arch of C1
and C2 (the spinolaminar line).
Lacking a body, the atlas is essentially a ring with
prominent articular processes that are appropriately
called lateral masses. The lateral masses divide the
ring into a smaller anterior and a larger posterior arch.
View C1-C2 cross section CT scan.
 On the inner aspects of the lateral masses are
tubercles for the transverse ligament that run between
these tubercles. The concave superior facets articulate
with the convex condyles of the occipital bone, while the
larger inferior facets (of C1) articulate with C2.
Because the atlas lacks a body, the lateral masses are
the major weight bearing structures, and a compression
force (axial load) can result in a bursting fracture of the
ring of C1. The upper CT image shows such fracture of
the C1 ring.
View odontoid view.
On the inner aspects of the lateral masses are
tubercles for the transverse ligament that run between
these tubercles. The concave superior facets articulate
with the convex condyles of the occipital bone, while the
larger inferior facets (of C1) articulate with C2.
Because the atlas lacks a body, the lateral masses are
the major weight bearing structures, and a compression
force (axial load) can result in a bursting fracture of the
ring of C1. The upper CT image shows such fracture of
the C1 ring.
View odontoid view.
 On an open-mouth odontoid view, the lateral
masses are easily visible as trapezoidal wedges. The
anterior and posterior arches are superimposed over
the odontoid process.
Radiographically, the surfaces of the anterior
atlantoaxial gap are parallel to each other and the
distance is less than 5 mm in a child. Widening of this
space can be a result of a transverse ligament tear,
allowing unstable motion between the two bones.
View lateral.
On an open-mouth odontoid view, the lateral
masses are easily visible as trapezoidal wedges. The
anterior and posterior arches are superimposed over
the odontoid process.
Radiographically, the surfaces of the anterior
atlantoaxial gap are parallel to each other and the
distance is less than 5 mm in a child. Widening of this
space can be a result of a transverse ligament tear,
allowing unstable motion between the two bones.
View lateral.
 On a lateral view, the atlas is a simple ring structure
seen edge on. The lateral masses are superimposed
on the odontoid process of C2 and are difficult to
identify. The inner aspect of the anterior arch can be
easily appreciated, as can the inner aspect of the
posterior arch. Note that the anterior arch articulates
with the anterior aspect of the odontoid, while the
posterior arch forms the very first posterior border of
the vertebral canal.
The most prominent feature of C2 (axis) is the
odontoid process, also called the dens. Both names
refer to its resemblance to a tooth. The odontoid
process projects superiorly from the body of the axis.
Articular processes centered around the odontoid have
smooth superior facets that facilitate rotational
articulation within the atlas. The inferior facets are
more posterior and in-line with the articular processes
of the rest of the cervical vertebrae area. On a lateral
view, the axis appears much like a typical cervical
vertebra, however, it is easily identified by the odontoid
process projecting vertically from the body and the large
and wide spinous process.
View odontoid view.
On a lateral view, the atlas is a simple ring structure
seen edge on. The lateral masses are superimposed
on the odontoid process of C2 and are difficult to
identify. The inner aspect of the anterior arch can be
easily appreciated, as can the inner aspect of the
posterior arch. Note that the anterior arch articulates
with the anterior aspect of the odontoid, while the
posterior arch forms the very first posterior border of
the vertebral canal.
The most prominent feature of C2 (axis) is the
odontoid process, also called the dens. Both names
refer to its resemblance to a tooth. The odontoid
process projects superiorly from the body of the axis.
Articular processes centered around the odontoid have
smooth superior facets that facilitate rotational
articulation within the atlas. The inferior facets are
more posterior and in-line with the articular processes
of the rest of the cervical vertebrae area. On a lateral
view, the axis appears much like a typical cervical
vertebra, however, it is easily identified by the odontoid
process projecting vertically from the body and the large
and wide spinous process.
View odontoid view.
 On an open-mouth odontoid view, the axis is shaped
like a fat bowling pin with wings. The odontoid and the
body form the bowling pin, and the articular processes
are the wings.
The articulation of the odontoid and the atlantal
anterior arch is unique. Anteriorly, it is between the two
bones; posteriorly, the dens articulates with the
transverse ligament that is attached to the inner
aspects of the atlantal lateral masses. The spinal cord
travels in the space posterior to the transverse
ligament.
View C1-C2 cross section CT scan.
On an open-mouth odontoid view, the axis is shaped
like a fat bowling pin with wings. The odontoid and the
body form the bowling pin, and the articular processes
are the wings.
The articulation of the odontoid and the atlantal
anterior arch is unique. Anteriorly, it is between the two
bones; posteriorly, the dens articulates with the
transverse ligament that is attached to the inner
aspects of the atlantal lateral masses. The spinal cord
travels in the space posterior to the transverse
ligament.
View C1-C2 cross section CT scan.
 The upper image is a CT scan axial image through
the ring of C1. The odontoid process is visible
anteriorly in the ring. The transverse ligament is not
easily visible on this CT cut; however, it is posterior to
the odontoid. The spinal cord is visible in the posterior
portion of the ring of C1 (the spinal canal). Note the
fracture in the anterior aspect of C1. The gap in the
posterior portion of C1 is a growth plate. Compare this
CT image with the bony model of C1 and C2.
View open mouth odontoid view.
The upper image is a CT scan axial image through
the ring of C1. The odontoid process is visible
anteriorly in the ring. The transverse ligament is not
easily visible on this CT cut; however, it is posterior to
the odontoid. The spinal cord is visible in the posterior
portion of the ring of C1 (the spinal canal). Note the
fracture in the anterior aspect of C1. The gap in the
posterior portion of C1 is a growth plate. Compare this
CT image with the bony model of C1 and C2.
View open mouth odontoid view.
 Developmentally, the bodies of the axis and the
dens arise from separate ossification centers. The
odontoid (dens) itself has three ossification centers.
There are two columnar centers, forming the body of
the odontoid that typically fuse before birth, and a
third center at the tip of the odontoid. During infancy,
before the tip of the odontoid has ossified, the
superior end of the odontoid may have a cleft in it
radiographically. The odontoid of children may have a
separate ossification center at the tip of the
odontoid--the os terminale. A finding of a fragment at
the superior-most tip of the odontoid may be due to a
fracture or it may a normal ossification pattern.
The most common normal radiographic pattern
mistaken for an odontoid fracture is the subdental
synchondrosis. This is a linear lucency at the base of
the dens. The dens usually fuses with the body of C2
somewhere between ages 3 and 6 years. However, a
thin, sclerotic "scar" of the synchondrosis may be
appreciable on the lateral view for many years
thereafter.
Normal laxity of the soft tissues of the
cervicocranium in the developing pediatric patient can
make radiologic interpretations more difficult. Laxity of
the prevertebral tissues can resemble abscesses,
hematomas, or tumors, particularly if the film is taken in
exhalation or in flexion. Laxity of the transverse atlantal
ligaments -- spanning from the dens to the inner aspect
of the lateral masses of the atlas -- allow greater range
of motion between these two bones. This, in addition to
the cartilaginous (non-ossified) nature of the outer
layers of the odontoid, accounts for an increased
anterior atlanto-odontoid (atlantodental) interval of 3-5
mm in infants. In addition, the margins of the anterior
atlanto-odontoid interval can lose their parallelism
during neck flexion. These pediatric norms can
resemble atlantoaxial subluxation. Furthermore, laxity
of the ligamentous structures around C3 can also
resemble subluxation at the C2-C3 or C3-C4 junctions.
Radiographic Views
The three most common views employed in the
emergency department are: 1) the lateral view, 2) the
AP view, and 3) the AP open mouth odontoid. The
lateral view can be taken as a cross-table lateral while
the patient is still on a spine board in the emergency
department. The anteroposterior views often require
transporting the patient to the imaging department.
Below is an introduction to reading these three common
views.
Lateral neck
The lateral cervical spine radiograph is the most
useful view. As many as 80-90% of cervical spine
injuries can be detected on the lateral view alone. The
quality of the film image obtained should be assessed.
All cervical vertebrae, C1-C7, and the top part of T1
should ideally be visible. It is important to be able to
count all 7 cervical and one thoracic vertebrae since the
most common lesions occur at the upper and lower
ends of the cervical spine. The most commonly missed
lesions occur at the C7-T1 junction simply because it is
not shown on the film.
To assess C-spine alignment, four imaginary lines
can be drawn on the lateral film; which aid evaluation of
vertebral alignment: 1) anterior longitudinal line, 2)
posterior longitudinal line, 3) posterior facet margins
(not shown on diagram), and 4) spinolaminar line.
View lateral.
Developmentally, the bodies of the axis and the
dens arise from separate ossification centers. The
odontoid (dens) itself has three ossification centers.
There are two columnar centers, forming the body of
the odontoid that typically fuse before birth, and a
third center at the tip of the odontoid. During infancy,
before the tip of the odontoid has ossified, the
superior end of the odontoid may have a cleft in it
radiographically. The odontoid of children may have a
separate ossification center at the tip of the
odontoid--the os terminale. A finding of a fragment at
the superior-most tip of the odontoid may be due to a
fracture or it may a normal ossification pattern.
The most common normal radiographic pattern
mistaken for an odontoid fracture is the subdental
synchondrosis. This is a linear lucency at the base of
the dens. The dens usually fuses with the body of C2
somewhere between ages 3 and 6 years. However, a
thin, sclerotic "scar" of the synchondrosis may be
appreciable on the lateral view for many years
thereafter.
Normal laxity of the soft tissues of the
cervicocranium in the developing pediatric patient can
make radiologic interpretations more difficult. Laxity of
the prevertebral tissues can resemble abscesses,
hematomas, or tumors, particularly if the film is taken in
exhalation or in flexion. Laxity of the transverse atlantal
ligaments -- spanning from the dens to the inner aspect
of the lateral masses of the atlas -- allow greater range
of motion between these two bones. This, in addition to
the cartilaginous (non-ossified) nature of the outer
layers of the odontoid, accounts for an increased
anterior atlanto-odontoid (atlantodental) interval of 3-5
mm in infants. In addition, the margins of the anterior
atlanto-odontoid interval can lose their parallelism
during neck flexion. These pediatric norms can
resemble atlantoaxial subluxation. Furthermore, laxity
of the ligamentous structures around C3 can also
resemble subluxation at the C2-C3 or C3-C4 junctions.
Radiographic Views
The three most common views employed in the
emergency department are: 1) the lateral view, 2) the
AP view, and 3) the AP open mouth odontoid. The
lateral view can be taken as a cross-table lateral while
the patient is still on a spine board in the emergency
department. The anteroposterior views often require
transporting the patient to the imaging department.
Below is an introduction to reading these three common
views.
Lateral neck
The lateral cervical spine radiograph is the most
useful view. As many as 80-90% of cervical spine
injuries can be detected on the lateral view alone. The
quality of the film image obtained should be assessed.
All cervical vertebrae, C1-C7, and the top part of T1
should ideally be visible. It is important to be able to
count all 7 cervical and one thoracic vertebrae since the
most common lesions occur at the upper and lower
ends of the cervical spine. The most commonly missed
lesions occur at the C7-T1 junction simply because it is
not shown on the film.
To assess C-spine alignment, four imaginary lines
can be drawn on the lateral film; which aid evaluation of
vertebral alignment: 1) anterior longitudinal line, 2)
posterior longitudinal line, 3) posterior facet margins
(not shown on diagram), and 4) spinolaminar line.
View lateral.
 The anterior and posterior longitudinal lines simply
correspond to the locations of the anterior and posterior
longitudinal ligaments. The spinolaminar line
demarcates the posterior limits of the spinal canal.
These lordotic contours should be smooth and without
step-offs.
The neck is normally positioned with lordosis
(extension). In adults, a straight C-spine (lack of
lordosis) indicates the presence of muscle spasm and a
possible occult fracture. In children, the absence of
lordosis is commonly seen. When positioned on a
spine board, the large occiput of most children positions
their neck in a straight (without lordosis) or in a flexed
alignment. This is common and does not necessarily
indicate the presence of a significant injury. However, it
does make interpretation of the radiographs more
difficult since such poor positioning may cause
artifact radiographic abnormalities.
Proper positioning of the atlantoaxial bones with the
occiput can be assessed by noting the alignment of two
imaginary lines. First, extension of a line down the
slope of the clivus should point to the superior end of
the dens (the os terminale). The posterior margin of the
foramen magnum should be in line with the
spinolaminar line. Such an alignment places the
foramen magnum in-line with the spinal canal, this
corresponds to the junction of the brain stem and the
spinal cord.
Dislocation of articular facets or a fractured
vertebrae may result in a discontinuity of the contours
of these lines with implications of instability and
decreased patency of the spinal canal lumen resulting
in impingement of the spinal cord.
Widening of the retropharyngeal space is a sign of
injury to either soft tissue or the adjacent vertebrae.
The retropharyngeal space (essentially, the
pre-vertebral soft tissue space) should be roughly half
the width of a vertebral body. Fractures of the C-spine
can result in hemorrhaging into the retropharyngeal
space, resulting in widening of this soft tissue space on
the lateral neck view.
The spacing of the facet joints, intervertebral
spaces, and interspinous gaps can provide hints to the
integrity of the mechanical stability of the connections
between vertebrae. The width of these spaces should
be fairly constant between sequential vertebrae. The
articular surfaces should be parallel to each other. In
addition, the spinous processes are generally
equidistant from each other but converge toward a point
at the base of the posterior neck. Pathologically,
increased spacing often results from tearing of the
supporting ligaments. Increased interspinous
distances, "fanning," is often associated with a posterior
longitudinal ligament tear. Decreased spacing could
lead to invagination of connective tissue into the spinal
canal.
The major features of all vertebra should be
examined. The height of each vertebral body should be
fairly constant from C3 through T1. A slight decrease in
height of a vertebral body may be a compression
fracture. A difference of greater than 25% can occur
only if the posterior intervertebral ligaments are torn.
The pedicles, facets, and laminae of each vertebra
should be superimposed upon each other in a properly
taken radiograph. Doubling of facets and articular
columns should be examined for evidence of unilateral
or bilateral dislocated facets.
The cortical surfaces of each vertebra should be
scrutinized for steps, breaks, or abnormal angulations.
Blurred edges may result from fractures or dislocations.
Often the tendons and ligaments are stronger than the
bones themselves, and tear-drop shaped pieces of
bone could be avulsed by a strong force acting on the
anterior longitudinal ligament. In the clay shoveller's
fracture (spinous process fracture), a downward force
on the supraspinous ligament shears most of the C6 or
C7 spinous process off its base.
AP View
The AP view is helpful in evaluating the vertical
alignment of the spinous processes and the
visualization of the vertebral body from the AP
perspective. This view is also important in evaluating
lateral displacement of fractures or entire vertebrae.
View AP.
The anterior and posterior longitudinal lines simply
correspond to the locations of the anterior and posterior
longitudinal ligaments. The spinolaminar line
demarcates the posterior limits of the spinal canal.
These lordotic contours should be smooth and without
step-offs.
The neck is normally positioned with lordosis
(extension). In adults, a straight C-spine (lack of
lordosis) indicates the presence of muscle spasm and a
possible occult fracture. In children, the absence of
lordosis is commonly seen. When positioned on a
spine board, the large occiput of most children positions
their neck in a straight (without lordosis) or in a flexed
alignment. This is common and does not necessarily
indicate the presence of a significant injury. However, it
does make interpretation of the radiographs more
difficult since such poor positioning may cause
artifact radiographic abnormalities.
Proper positioning of the atlantoaxial bones with the
occiput can be assessed by noting the alignment of two
imaginary lines. First, extension of a line down the
slope of the clivus should point to the superior end of
the dens (the os terminale). The posterior margin of the
foramen magnum should be in line with the
spinolaminar line. Such an alignment places the
foramen magnum in-line with the spinal canal, this
corresponds to the junction of the brain stem and the
spinal cord.
Dislocation of articular facets or a fractured
vertebrae may result in a discontinuity of the contours
of these lines with implications of instability and
decreased patency of the spinal canal lumen resulting
in impingement of the spinal cord.
Widening of the retropharyngeal space is a sign of
injury to either soft tissue or the adjacent vertebrae.
The retropharyngeal space (essentially, the
pre-vertebral soft tissue space) should be roughly half
the width of a vertebral body. Fractures of the C-spine
can result in hemorrhaging into the retropharyngeal
space, resulting in widening of this soft tissue space on
the lateral neck view.
The spacing of the facet joints, intervertebral
spaces, and interspinous gaps can provide hints to the
integrity of the mechanical stability of the connections
between vertebrae. The width of these spaces should
be fairly constant between sequential vertebrae. The
articular surfaces should be parallel to each other. In
addition, the spinous processes are generally
equidistant from each other but converge toward a point
at the base of the posterior neck. Pathologically,
increased spacing often results from tearing of the
supporting ligaments. Increased interspinous
distances, "fanning," is often associated with a posterior
longitudinal ligament tear. Decreased spacing could
lead to invagination of connective tissue into the spinal
canal.
The major features of all vertebra should be
examined. The height of each vertebral body should be
fairly constant from C3 through T1. A slight decrease in
height of a vertebral body may be a compression
fracture. A difference of greater than 25% can occur
only if the posterior intervertebral ligaments are torn.
The pedicles, facets, and laminae of each vertebra
should be superimposed upon each other in a properly
taken radiograph. Doubling of facets and articular
columns should be examined for evidence of unilateral
or bilateral dislocated facets.
The cortical surfaces of each vertebra should be
scrutinized for steps, breaks, or abnormal angulations.
Blurred edges may result from fractures or dislocations.
Often the tendons and ligaments are stronger than the
bones themselves, and tear-drop shaped pieces of
bone could be avulsed by a strong force acting on the
anterior longitudinal ligament. In the clay shoveller's
fracture (spinous process fracture), a downward force
on the supraspinous ligament shears most of the C6 or
C7 spinous process off its base.
AP View
The AP view is helpful in evaluating the vertical
alignment of the spinous processes and the
visualization of the vertebral body from the AP
perspective. This view is also important in evaluating
lateral displacement of fractures or entire vertebrae.
View AP.
 Typically, in this view, the mandible and occiput are
superimposed over C1 and C2, and sometimes the
upper portions of C3 may be obscured. An adequate
film should clearly show the vertebral column from C3
to T1.
Spinous processes should be aligned in the midline
and be generally equidistant from one another.
Misalignment of the spinous processes may suggest a
dislocation or a fracture of an articular surface.
Increased spacing between spinous processes or an
apparent missing spinous process in this view may
suggest a fractured spinous process, as in the clay
shoveller's fracture (spinous process fracture). A
widened gap may also be due to a tear of the posterior
longitudinal ligament, resulting in "fanning" as seen on a
lateral radiograph.
The trachea is easily visualized in this view.
Disruption of tracheal radiolucency may also indicate
nearby lesions.
The intervertebral spaces should be evaluated for
uniformity from one vertebral pair to another. The
spaces should be of similar distances apart and the
articular surfaces should be fairly parallel to each other.
Dislocations and ligamentous tears may produce
widened or narrowed joint spaces in an AP view.
Lastly, the vertebrae should be evaluated for
fractures. The cortical surfaces should be continuous
and well defined. Each vertebral body should be
rectangular and of similar size. The uncinate
processes (U), bilateral raised lips on the superior
surface of the vertebral bodies, are most easily
evaluated for fractures from this AP view.
Open-Mouth Odontoid View
The AP open-mouth odontoid radiograph is used to
evaluate the cervicocranium from another perspective.
It is most valuable in assessing the relationship
between the lateral masses of the atlas and the axis.
The junction between C1 and C2 should be clearly
visible. Visibility of the entire odontoid process is of
secondary importance.
View odontoid view.
Typically, in this view, the mandible and occiput are
superimposed over C1 and C2, and sometimes the
upper portions of C3 may be obscured. An adequate
film should clearly show the vertebral column from C3
to T1.
Spinous processes should be aligned in the midline
and be generally equidistant from one another.
Misalignment of the spinous processes may suggest a
dislocation or a fracture of an articular surface.
Increased spacing between spinous processes or an
apparent missing spinous process in this view may
suggest a fractured spinous process, as in the clay
shoveller's fracture (spinous process fracture). A
widened gap may also be due to a tear of the posterior
longitudinal ligament, resulting in "fanning" as seen on a
lateral radiograph.
The trachea is easily visualized in this view.
Disruption of tracheal radiolucency may also indicate
nearby lesions.
The intervertebral spaces should be evaluated for
uniformity from one vertebral pair to another. The
spaces should be of similar distances apart and the
articular surfaces should be fairly parallel to each other.
Dislocations and ligamentous tears may produce
widened or narrowed joint spaces in an AP view.
Lastly, the vertebrae should be evaluated for
fractures. The cortical surfaces should be continuous
and well defined. Each vertebral body should be
rectangular and of similar size. The uncinate
processes (U), bilateral raised lips on the superior
surface of the vertebral bodies, are most easily
evaluated for fractures from this AP view.
Open-Mouth Odontoid View
The AP open-mouth odontoid radiograph is used to
evaluate the cervicocranium from another perspective.
It is most valuable in assessing the relationship
between the lateral masses of the atlas and the axis.
The junction between C1 and C2 should be clearly
visible. Visibility of the entire odontoid process is of
secondary importance.
View odontoid view.
 From this perspective, left and right symmetry is
most helpful in evaluation. The two atlantal lateral
masses should be equidistant from the dens, and the
articular surfaces of the atlantoaxial lateral masses
should be in perfect alignment. The inferior facets of
the atlantal (C1) lateral masses should be parallel to
and aligned with the upper facets of the axial (C2)
lateral masses (white arrows point to the lateral margin
of the facet joint). Lateral displacement of one or both
of the atlantal lateral masses (black arrow) is
suggestive of a Jefferson fracture in which the ring of
C1 is fractured, bursting it open displacing the lateral
masses outward.
The lateral masses should also be scrutinized for
unequal size. In rotary subluxation, the atlas is turned
such that one lateral mass is farther than the other from
the radiographic film and may appear larger. However,
rotary subluxation is best confirmed on a CT scan.
Laxity of ligamentous attachments surrounding the
odontoid and incomplete ossification of the odontoid
may allow up to two-thirds of the anterior atlantal arch
to be above the tip of the odontoid process.
Fractures of the odontoid are common and can be
seen on lateral and open-mouth odontoid views. These
fractures are classified according to the location of the
fracture. Type I is an oblique fracture through the upper
portion of the odontoid. It should be noted that
sometimes the upper incisors can obscure portions of
the upper odontoid and simulate a Type I fracture.
Type II fractures occur at the base of the odontoid
where it joins the body of C2. This is the most common
odontoid fracture. Unfortunately, this is also the
location of the subdental synchondrosis.
NOTE: While it is not unusual for the odontoid to be
tilted posteriorly, it should NOT be tilted anteriorly. This
is more indicative of an odontoid fracture. Widening of
the subdental synchondrosis coupled with anterior tilting
of the odontoid are highly indicative of an odontoid
fracture.
A Type III odontoid fracture extends into the
vertebral body of C2.
The odontoid image shows three open mouth
odontoid radiographs on the right. The upper
radiograph shows the odontoid well. However, the
lateral margins of the lateral masses of C1 and C2 are
obscured by the patient's lower teeth, making it
impossible to assess the lateral alignment of the C1-C2
facet joints.
The middle image shows a bursting ring fracture of
C1 with outward displacement of the C1 lateral masses
(black arrow). The lower image shows normal
alignment of the C1-C2 facet joints. The white arrow
points to the lateral margin of the facet joint.
Other Special Views
In addition to the standard three views (lateral, AP,
odontoid), other radiographic views can aid in obtaining
a better perspective on a suspected lesion.
Swimmer's View: Recall that an adequate lateral
film should reveal all seven cervical vertebrae and
upper T1. Typically, downward traction on the arms will
produce the adequate visualization in most cases.
Should the C7/T1 junction still be obscured, a
swimmer's view can be obtained by elevating the arm
closest to the film. This posture yields a slightly oblique
view of the vertebral column, but moves the shoulder
joint above the C7/T1 junction. C7/T1 can easily be
seen in this view; however, it is often overlapping with
dense soft tissue and the bones of the shoulder.
View swimmer's view.
From this perspective, left and right symmetry is
most helpful in evaluation. The two atlantal lateral
masses should be equidistant from the dens, and the
articular surfaces of the atlantoaxial lateral masses
should be in perfect alignment. The inferior facets of
the atlantal (C1) lateral masses should be parallel to
and aligned with the upper facets of the axial (C2)
lateral masses (white arrows point to the lateral margin
of the facet joint). Lateral displacement of one or both
of the atlantal lateral masses (black arrow) is
suggestive of a Jefferson fracture in which the ring of
C1 is fractured, bursting it open displacing the lateral
masses outward.
The lateral masses should also be scrutinized for
unequal size. In rotary subluxation, the atlas is turned
such that one lateral mass is farther than the other from
the radiographic film and may appear larger. However,
rotary subluxation is best confirmed on a CT scan.
Laxity of ligamentous attachments surrounding the
odontoid and incomplete ossification of the odontoid
may allow up to two-thirds of the anterior atlantal arch
to be above the tip of the odontoid process.
Fractures of the odontoid are common and can be
seen on lateral and open-mouth odontoid views. These
fractures are classified according to the location of the
fracture. Type I is an oblique fracture through the upper
portion of the odontoid. It should be noted that
sometimes the upper incisors can obscure portions of
the upper odontoid and simulate a Type I fracture.
Type II fractures occur at the base of the odontoid
where it joins the body of C2. This is the most common
odontoid fracture. Unfortunately, this is also the
location of the subdental synchondrosis.
NOTE: While it is not unusual for the odontoid to be
tilted posteriorly, it should NOT be tilted anteriorly. This
is more indicative of an odontoid fracture. Widening of
the subdental synchondrosis coupled with anterior tilting
of the odontoid are highly indicative of an odontoid
fracture.
A Type III odontoid fracture extends into the
vertebral body of C2.
The odontoid image shows three open mouth
odontoid radiographs on the right. The upper
radiograph shows the odontoid well. However, the
lateral margins of the lateral masses of C1 and C2 are
obscured by the patient's lower teeth, making it
impossible to assess the lateral alignment of the C1-C2
facet joints.
The middle image shows a bursting ring fracture of
C1 with outward displacement of the C1 lateral masses
(black arrow). The lower image shows normal
alignment of the C1-C2 facet joints. The white arrow
points to the lateral margin of the facet joint.
Other Special Views
In addition to the standard three views (lateral, AP,
odontoid), other radiographic views can aid in obtaining
a better perspective on a suspected lesion.
Swimmer's View: Recall that an adequate lateral
film should reveal all seven cervical vertebrae and
upper T1. Typically, downward traction on the arms will
produce the adequate visualization in most cases.
Should the C7/T1 junction still be obscured, a
swimmer's view can be obtained by elevating the arm
closest to the film. This posture yields a slightly oblique
view of the vertebral column, but moves the shoulder
joint above the C7/T1 junction. C7/T1 can easily be
seen in this view; however, it is often overlapping with
dense soft tissue and the bones of the shoulder.
View swimmer's view.
 In this swimmer's view, note that the lower cervical
spine can be seen, but in this case, it is still not optimal
since C7 is still not visualized.
Oblique Projections: The oblique views provide
good visualization of the posterior structures of the
vertebral column, such as the intervertebral foramina
and articulation of the facets. They are particularly
helpful in evaluating suspected unilateral facet
dislocations since only one half of the facets and
intervertebral foramina are viewed at a time. The
foramina are also best visualized on these views.
View oblique views.
In this swimmer's view, note that the lower cervical
spine can be seen, but in this case, it is still not optimal
since C7 is still not visualized.
Oblique Projections: The oblique views provide
good visualization of the posterior structures of the
vertebral column, such as the intervertebral foramina
and articulation of the facets. They are particularly
helpful in evaluating suspected unilateral facet
dislocations since only one half of the facets and
intervertebral foramina are viewed at a time. The
foramina are also best visualized on these views.
View oblique views.
 Lateral Flexion and Extension Views: The flexion
and extension views are obtained on a conscious
patient who can actively bend their neck. Care must be
taken in obtaining these views as there is risk of further
displacement. In appropriate circumstances, these
views may be particularly helpful in excluding
ligamentous injury and potential instability. Some
physicians have found the flexion view invaluable in
detecting occult posterior ligamentous injuries resulting
from hyperflexion.
References
1. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - I. BMJ
Sept1993;307(25):785-789.
2. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - II. BMJ
Oct1993:307(2):855-859.
3. Ellis GL. Imaging of the Atlas (C1) and Axis
(C2). Emergency Medicine Clinics of North America.
1991;9(4):719-731.
4. Gerlock AJ, et al. Advanced Excercises in
Diagnositic Radiology - 11: The Cervical Spine in
Trauma. Philadelphia, W. B. Saunders Company,
1978.
5. Goldberg S. Clinical Anatomy made Ridiculously
Simple. Miami, MedMaster, Inc. 1986.
6. Harris JH, Mirvis SE. The Radiology of Acute
Cervical Spine Trauma, Third Edition. Baltimore,
Williams & Wilkins, 1996, pp.1-72, 86, 180-196.
7. Montgomery JL, Montgomery ML. Radiographic
evaluation ofcervical spine trauma: Procedures to avoid
catastrophe. Postgrad Med 1994;95(4):173-196.
8. Moore KL. Clinically Oriented Anatomy, Second
Edition. Baltimore, Williams & Wilkins, 1985, pp.
576-578, 585-596.
9. Netter FH. Atlas of Human Anatomy. Summit:
Ciba-GeigyCorporation, 1989. Plates 12-16, 30, 57, 59,
172.
10. Swisschuk LE. Emergency Imaging of The
Acutely Ill or Injured Child, Third Edition. Baltimore,
Williams & Wilkins, 1994, pp.653-717.
11. Walsh-Kelly CM, et al. Clinical impact of
radiograph misinterpretation in a pediatric ED and the
effect of physician training level. Am J Emerg Med
1995;13(3): 262-264.
12. Harris JH, Harris WH, Novelline RA. The
Radiology of Emergency Medicine, third edition.
Baltimore, Williams & WIlkins, 1993, pp. 127-244.
Lateral Flexion and Extension Views: The flexion
and extension views are obtained on a conscious
patient who can actively bend their neck. Care must be
taken in obtaining these views as there is risk of further
displacement. In appropriate circumstances, these
views may be particularly helpful in excluding
ligamentous injury and potential instability. Some
physicians have found the flexion view invaluable in
detecting occult posterior ligamentous injuries resulting
from hyperflexion.
References
1. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - I. BMJ
Sept1993;307(25):785-789.
2. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - II. BMJ
Oct1993:307(2):855-859.
3. Ellis GL. Imaging of the Atlas (C1) and Axis
(C2). Emergency Medicine Clinics of North America.
1991;9(4):719-731.
4. Gerlock AJ, et al. Advanced Excercises in
Diagnositic Radiology - 11: The Cervical Spine in
Trauma. Philadelphia, W. B. Saunders Company,
1978.
5. Goldberg S. Clinical Anatomy made Ridiculously
Simple. Miami, MedMaster, Inc. 1986.
6. Harris JH, Mirvis SE. The Radiology of Acute
Cervical Spine Trauma, Third Edition. Baltimore,
Williams & Wilkins, 1996, pp.1-72, 86, 180-196.
7. Montgomery JL, Montgomery ML. Radiographic
evaluation ofcervical spine trauma: Procedures to avoid
catastrophe. Postgrad Med 1994;95(4):173-196.
8. Moore KL. Clinically Oriented Anatomy, Second
Edition. Baltimore, Williams & Wilkins, 1985, pp.
576-578, 585-596.
9. Netter FH. Atlas of Human Anatomy. Summit:
Ciba-GeigyCorporation, 1989. Plates 12-16, 30, 57, 59,
172.
10. Swisschuk LE. Emergency Imaging of The
Acutely Ill or Injured Child, Third Edition. Baltimore,
Williams & Wilkins, 1994, pp.653-717.
11. Walsh-Kelly CM, et al. Clinical impact of
radiograph misinterpretation in a pediatric ED and the
effect of physician training level. Am J Emerg Med
1995;13(3): 262-264.
12. Harris JH, Harris WH, Novelline RA. The
Radiology of Emergency Medicine, third edition.
Baltimore, Williams & WIlkins, 1993, pp. 127-244.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 The three line diagrams on the left from top to
bottom include an axial view, viewed from the top (Top),
an anterior view (AP), and a lateral view (Lat). The
three photographs of C4 on the right from top to bottom
include a view from the top (Top), a view from the
bottom (Bottom), and an oblique view from the bottom
(Bottom oblique).
Identify the following structures on these diagrams
and photos:
SP - spinous process
L - lamina (forms roof of the neural arch)
P - pedicle (forms supports of the neural arch)
SC - spinal canal
VB - vertebral body
SAF - superior articular facet
IAF - inferior articular facet
TF - transverse foramen
Gr - groove for spinal nerve (transverse process)
U - uncinate process
The neural arch is formed by the laminae, the base
of the spinous process and the pedicles. The pedicles
are very short in the cervical spine. The facet joints are
formed by the inferior and superior facets such that the
C4-C5 facet joint is formed by the inferior articular facet
of C4 and the superior articular facet of C5.
On a lateral film, the body is a rhomboid with the
posterior portion slightly taller than the anterior portion.
View lateral C-spine view.
The three line diagrams on the left from top to
bottom include an axial view, viewed from the top (Top),
an anterior view (AP), and a lateral view (Lat). The
three photographs of C4 on the right from top to bottom
include a view from the top (Top), a view from the
bottom (Bottom), and an oblique view from the bottom
(Bottom oblique).
Identify the following structures on these diagrams
and photos:
SP - spinous process
L - lamina (forms roof of the neural arch)
P - pedicle (forms supports of the neural arch)
SC - spinal canal
VB - vertebral body
SAF - superior articular facet
IAF - inferior articular facet
TF - transverse foramen
Gr - groove for spinal nerve (transverse process)
U - uncinate process
The neural arch is formed by the laminae, the base
of the spinous process and the pedicles. The pedicles
are very short in the cervical spine. The facet joints are
formed by the inferior and superior facets such that the
C4-C5 facet joint is formed by the inferior articular facet
of C4 and the superior articular facet of C5.
On a lateral film, the body is a rhomboid with the
posterior portion slightly taller than the anterior portion.
View lateral C-spine view.
 The lateral view of a very young child is shown on
the left compared to the lateral view of a teenager on
the right. Alignment is assessed by the integrity of lines
drawn along: 1) the anterior borders of the vertebral
bodies, 2) the posterior borders of the vertebral bodies
and 3) the anterior borders of the vertebral arch's apex
(spinolaminal line). The facet joints should be clearly
visible.
View identifying landmarks.
The lateral view of a very young child is shown on
the left compared to the lateral view of a teenager on
the right. Alignment is assessed by the integrity of lines
drawn along: 1) the anterior borders of the vertebral
bodies, 2) the posterior borders of the vertebral bodies
and 3) the anterior borders of the vertebral arch's apex
(spinolaminal line). The facet joints should be clearly
visible.
View identifying landmarks.
 The contour lines of alignment are shown. Identify
the following areas on the radiographs:
F - facet joint
SP - spinous process
L - lamina
Od - odontoid
On an AP view, the lateral superior edges of the
body form bilateral ridges, called the uncinate
processes (U).
View AP C-spine view.
The contour lines of alignment are shown. Identify
the following areas on the radiographs:
F - facet joint
SP - spinous process
L - lamina
Od - odontoid
On an AP view, the lateral superior edges of the
body form bilateral ridges, called the uncinate
processes (U).
View AP C-spine view.
 A posterior view of the cervical spine is shown on
the left. An anterior view is shown in the center.
Axial compression can result in compression
fractures which can lead to decreased vertebral body
height or a burst fracture that fragments the vertebral
body. A strong lateral force can cause a shearing
action and create fractures of an uncinate process.
Hyperflexion and hyperextension may also result in
teardrop fractures of the anterior superior or inferior
corner of the body.
Between the vertebral bodies are the intervertebral
disks. These function as shock absorbers. As in the
lumbar region, rupture of the annulus can lead to
encroachment into the spinal canal. The vertebral body
also serves as the attachment site of the anterior and
posterior longitudinal ligaments. Tears in these
ligamentous structures can result from displacement or
extensive fractures of the vertebral body. Without
these ligamentous connections, the vertebral column is
unstable.
Neural Arch
Posterior to the vertebral body is the neural arch
(vertebral arch covering the spinal canal). The neural
arch refers to all the structures dorsal to the body. The
arch serves to protect the spinal cord, provide
attachment sites for ligaments and muscles, and forms
synovial joints that facilitate movement of the vertebral
column. The major structures that make up the arch
include: 1) the pedicles, 2) the laminae, 3) the spinous
process, 4) the articular processes and facets, and 5)
the transverse processes.
View C4.
A posterior view of the cervical spine is shown on
the left. An anterior view is shown in the center.
Axial compression can result in compression
fractures which can lead to decreased vertebral body
height or a burst fracture that fragments the vertebral
body. A strong lateral force can cause a shearing
action and create fractures of an uncinate process.
Hyperflexion and hyperextension may also result in
teardrop fractures of the anterior superior or inferior
corner of the body.
Between the vertebral bodies are the intervertebral
disks. These function as shock absorbers. As in the
lumbar region, rupture of the annulus can lead to
encroachment into the spinal canal. The vertebral body
also serves as the attachment site of the anterior and
posterior longitudinal ligaments. Tears in these
ligamentous structures can result from displacement or
extensive fractures of the vertebral body. Without
these ligamentous connections, the vertebral column is
unstable.
Neural Arch
Posterior to the vertebral body is the neural arch
(vertebral arch covering the spinal canal). The neural
arch refers to all the structures dorsal to the body. The
arch serves to protect the spinal cord, provide
attachment sites for ligaments and muscles, and forms
synovial joints that facilitate movement of the vertebral
column. The major structures that make up the arch
include: 1) the pedicles, 2) the laminae, 3) the spinous
process, 4) the articular processes and facets, and 5)
the transverse processes.
View C4.
 Pedicles
The pedicles ("little feet") form the supports of the
neural arch as it is attached to the vertebral body. In
the cervical spine, the pedicles are short. They project
posteriorly (dorsally) from the body and form the lateral
borders of the spinal canal. Superior and slightly larger
inferior vertebral notches above and below the pedicles
form intervertebral foramina in the articulated vertebral
column. Through these foramina pass the cervical
spinal nerves.
View lateral.
Pedicles
The pedicles ("little feet") form the supports of the
neural arch as it is attached to the vertebral body. In
the cervical spine, the pedicles are short. They project
posteriorly (dorsally) from the body and form the lateral
borders of the spinal canal. Superior and slightly larger
inferior vertebral notches above and below the pedicles
form intervertebral foramina in the articulated vertebral
column. Through these foramina pass the cervical
spinal nerves.
View lateral.
 On a lateral film, the pedicles appear as small
connections between the body and the articular
processes (see below). On the AP view, the pedicles
appear as small doughnut densities on the lateral upper
portion of the vertebral body, just below the uncinate
processes. Fractures in this region can disrupt the
spinal nerves or the spinal cord itself.
View AP.
On a lateral film, the pedicles appear as small
connections between the body and the articular
processes (see below). On the AP view, the pedicles
appear as small doughnut densities on the lateral upper
portion of the vertebral body, just below the uncinate
processes. Fractures in this region can disrupt the
spinal nerves or the spinal cord itself.
View AP.
 Laminae
The laminae (meaning "layers") form a roof over
the neural arch, supported by the pedicles. In addition
to the obvious protective function, the laminae also
serve as the site of attachment for the ligamentum
flavum. Because the laminae are thinner in the C-spine
compared to other vertebrae, their relative radiolucency
appears as an apparent gap between the posterior
cortex of the articular facets and the anterior cortex of
the spinous process (posterior aspect of the neural
arch) on the lateral view. In general, the laminae (L)
are not easily appreciable on an AP view.
View lateral.
Laminae
The laminae (meaning "layers") form a roof over
the neural arch, supported by the pedicles. In addition
to the obvious protective function, the laminae also
serve as the site of attachment for the ligamentum
flavum. Because the laminae are thinner in the C-spine
compared to other vertebrae, their relative radiolucency
appears as an apparent gap between the posterior
cortex of the articular facets and the anterior cortex of
the spinous process (posterior aspect of the neural
arch) on the lateral view. In general, the laminae (L)
are not easily appreciable on an AP view.
View lateral.
 Spinous Process
The spinous process projects dorsoinferiorly from
the point of union of the laminae. Unique to the typical
cervical vertebrae, the spinous processes of C3 through
C6 are typically bifid at the tips. The spine of C7 is an
easily visible surface landmark called the vertebra
prominens. The spinous processes are the site of
attachment for a number of ligamentous and tendinous
structures. The major ligaments associated with the
spine include the interspinous and supraspinous
ligaments as well as the ligamentum nuchae. A number
of intrinsic muscles of the spine as well as large back
muscles such as the trapezius, the levator scapularis,
and the rhomboids are attached to the cervical spinous
processes. Excessive load on these muscles may
result in avulsion of the spinous processes of C6 and
C7, commonly known as the clay shoveller's fracture.
This fracture is more commonly found in adults.
View lateral.
Spinous Process
The spinous process projects dorsoinferiorly from
the point of union of the laminae. Unique to the typical
cervical vertebrae, the spinous processes of C3 through
C6 are typically bifid at the tips. The spine of C7 is an
easily visible surface landmark called the vertebra
prominens. The spinous processes are the site of
attachment for a number of ligamentous and tendinous
structures. The major ligaments associated with the
spine include the interspinous and supraspinous
ligaments as well as the ligamentum nuchae. A number
of intrinsic muscles of the spine as well as large back
muscles such as the trapezius, the levator scapularis,
and the rhomboids are attached to the cervical spinous
processes. Excessive load on these muscles may
result in avulsion of the spinous processes of C6 and
C7, commonly known as the clay shoveller's fracture.
This fracture is more commonly found in adults.
View lateral.
 On a lateral view, the spinous processes appear as
triangular extensions. The anterior border with the
laminae (spinolaminal line) is an easily visible feature
marking the posterior border of the vertebral canal
(spinal canal). On an AP view, the spinous processes
appear as a midline density superimposed on the
vertebral body. The bifid nature of some of the cervical
spines can be easily appreciated in this view.
View AP.
On a lateral view, the spinous processes appear as
triangular extensions. The anterior border with the
laminae (spinolaminal line) is an easily visible feature
marking the posterior border of the vertebral canal
(spinal canal). On an AP view, the spinous processes
appear as a midline density superimposed on the
vertebral body. The bifid nature of some of the cervical
spines can be easily appreciated in this view.
View AP.
 Articular Processes and Articular Facets
The articular processes are cylindrical structures at
the junction of the pedicles and the laminae. Like the
pedicles, articular processes also delimit the lateral
margins of the spinal canal. The articular facets, the
oblique elliptical ends of the cylinders, are higher
anteriorly and lower posteriorly.
View articular facets of C4.
Articular Processes and Articular Facets
The articular processes are cylindrical structures at
the junction of the pedicles and the laminae. Like the
pedicles, articular processes also delimit the lateral
margins of the spinal canal. The articular facets, the
oblique elliptical ends of the cylinders, are higher
anteriorly and lower posteriorly.
View articular facets of C4.
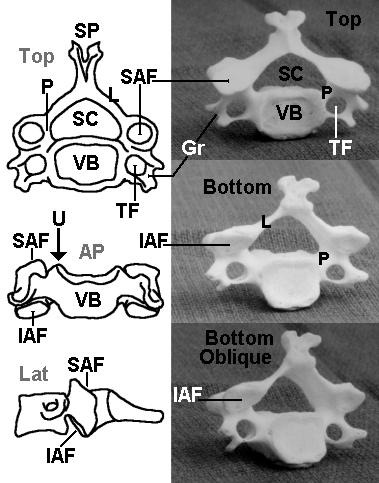 Capsular articular ligaments join adjacent inferior
and superior articular facets of successive vertebrae to
form synovial joints. Strong rotary forces can stretch or
tear these ligaments resulting in unilateral or bilateral
dislocated facets.
View lateral.
Capsular articular ligaments join adjacent inferior
and superior articular facets of successive vertebrae to
form synovial joints. Strong rotary forces can stretch or
tear these ligaments resulting in unilateral or bilateral
dislocated facets.
View lateral.
 On a lateral view, the articular processes are
rhomboidal in shape and superimposed upon one
another. Unlike the vertebral body which slopes
downward anteriorly, the articular processes slope
sharply downward posteriorly. They appear
superimposed on the spinal canal.
View oblique view.
On a lateral view, the articular processes are
rhomboidal in shape and superimposed upon one
another. Unlike the vertebral body which slopes
downward anteriorly, the articular processes slope
sharply downward posteriorly. They appear
superimposed on the spinal canal.
View oblique view.
 The skeletal model on the left shows variability in
the intervertebral disk spacing due to poor positioning of
the model bones during photography. This oblique view
shows the intervertebral foramina formed by the inferior
notch of the pedicle of the vertebrae above and the
superior notch of the pedicle of the vertebrae below.
Transverse Processes
The transverse processes project outward
anteroinferiorly from the pedicles like half-cylindrical
scoops.
View C4.
The skeletal model on the left shows variability in
the intervertebral disk spacing due to poor positioning of
the model bones during photography. This oblique view
shows the intervertebral foramina formed by the inferior
notch of the pedicle of the vertebrae above and the
superior notch of the pedicle of the vertebrae below.
Transverse Processes
The transverse processes project outward
anteroinferiorly from the pedicles like half-cylindrical
scoops.
View C4.
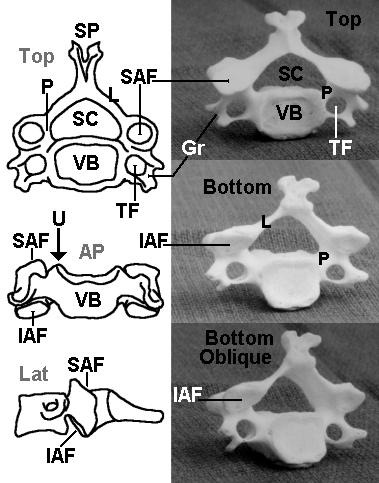 Along the grooved portion of the transverse
process pass the ventral rami of the cervical nerves.
The dorsal rami pass more posteriorly. In the middle
of the transverse process is a foramen for the vertebral
artery as it courses upward toward the foramen
magnum. Lesions in this region can damage the
nerves of cervical and brachial plexi as well as
compromise the arterial supply of the posterior brain.
The Cervicocranium
The articulations between the occiput, the atlas
(C1), and the axis (C2) are highly specialized to allow
the extensive range of motion of the head upon the
neck. As such, C1 and C2 differ sufficiently from the
typical vertebrae that they deserve special mention.
View odontoid view.
Along the grooved portion of the transverse
process pass the ventral rami of the cervical nerves.
The dorsal rami pass more posteriorly. In the middle
of the transverse process is a foramen for the vertebral
artery as it courses upward toward the foramen
magnum. Lesions in this region can damage the
nerves of cervical and brachial plexi as well as
compromise the arterial supply of the posterior brain.
The Cervicocranium
The articulations between the occiput, the atlas
(C1), and the axis (C2) are highly specialized to allow
the extensive range of motion of the head upon the
neck. As such, C1 and C2 differ sufficiently from the
typical vertebrae that they deserve special mention.
View odontoid view.
 The atlas (C1) articulates superiorly with the
occipital bone. The occipital bone forms the base of the
cranium, and articulation with the cervical spine is via
the pair of large convex occipital condyles situated on
either side of the anterior half of the foramen magnum.
The brain stem becomes the spinal cord as it leaves the
cranium through the foramen magnum. Anterior to the
foramen magnum is an upward incline to the dorsum
sellae called the clivus. The posterior aspect of the
foramen magnum is in-line with the posterior arch of C1
and C2 (the spinolaminar line).
Lacking a body, the atlas is essentially a ring with
prominent articular processes that are appropriately
called lateral masses. The lateral masses divide the
ring into a smaller anterior and a larger posterior arch.
View C1-C2 cross section CT scan.
The atlas (C1) articulates superiorly with the
occipital bone. The occipital bone forms the base of the
cranium, and articulation with the cervical spine is via
the pair of large convex occipital condyles situated on
either side of the anterior half of the foramen magnum.
The brain stem becomes the spinal cord as it leaves the
cranium through the foramen magnum. Anterior to the
foramen magnum is an upward incline to the dorsum
sellae called the clivus. The posterior aspect of the
foramen magnum is in-line with the posterior arch of C1
and C2 (the spinolaminar line).
Lacking a body, the atlas is essentially a ring with
prominent articular processes that are appropriately
called lateral masses. The lateral masses divide the
ring into a smaller anterior and a larger posterior arch.
View C1-C2 cross section CT scan.
 On the inner aspects of the lateral masses are
tubercles for the transverse ligament that run between
these tubercles. The concave superior facets articulate
with the convex condyles of the occipital bone, while the
larger inferior facets (of C1) articulate with C2.
Because the atlas lacks a body, the lateral masses are
the major weight bearing structures, and a compression
force (axial load) can result in a bursting fracture of the
ring of C1. The upper CT image shows such fracture of
the C1 ring.
View odontoid view.
On the inner aspects of the lateral masses are
tubercles for the transverse ligament that run between
these tubercles. The concave superior facets articulate
with the convex condyles of the occipital bone, while the
larger inferior facets (of C1) articulate with C2.
Because the atlas lacks a body, the lateral masses are
the major weight bearing structures, and a compression
force (axial load) can result in a bursting fracture of the
ring of C1. The upper CT image shows such fracture of
the C1 ring.
View odontoid view.
 On an open-mouth odontoid view, the lateral
masses are easily visible as trapezoidal wedges. The
anterior and posterior arches are superimposed over
the odontoid process.
Radiographically, the surfaces of the anterior
atlantoaxial gap are parallel to each other and the
distance is less than 5 mm in a child. Widening of this
space can be a result of a transverse ligament tear,
allowing unstable motion between the two bones.
View lateral.
On an open-mouth odontoid view, the lateral
masses are easily visible as trapezoidal wedges. The
anterior and posterior arches are superimposed over
the odontoid process.
Radiographically, the surfaces of the anterior
atlantoaxial gap are parallel to each other and the
distance is less than 5 mm in a child. Widening of this
space can be a result of a transverse ligament tear,
allowing unstable motion between the two bones.
View lateral.
 On a lateral view, the atlas is a simple ring structure
seen edge on. The lateral masses are superimposed
on the odontoid process of C2 and are difficult to
identify. The inner aspect of the anterior arch can be
easily appreciated, as can the inner aspect of the
posterior arch. Note that the anterior arch articulates
with the anterior aspect of the odontoid, while the
posterior arch forms the very first posterior border of
the vertebral canal.
The most prominent feature of C2 (axis) is the
odontoid process, also called the dens. Both names
refer to its resemblance to a tooth. The odontoid
process projects superiorly from the body of the axis.
Articular processes centered around the odontoid have
smooth superior facets that facilitate rotational
articulation within the atlas. The inferior facets are
more posterior and in-line with the articular processes
of the rest of the cervical vertebrae area. On a lateral
view, the axis appears much like a typical cervical
vertebra, however, it is easily identified by the odontoid
process projecting vertically from the body and the large
and wide spinous process.
View odontoid view.
On a lateral view, the atlas is a simple ring structure
seen edge on. The lateral masses are superimposed
on the odontoid process of C2 and are difficult to
identify. The inner aspect of the anterior arch can be
easily appreciated, as can the inner aspect of the
posterior arch. Note that the anterior arch articulates
with the anterior aspect of the odontoid, while the
posterior arch forms the very first posterior border of
the vertebral canal.
The most prominent feature of C2 (axis) is the
odontoid process, also called the dens. Both names
refer to its resemblance to a tooth. The odontoid
process projects superiorly from the body of the axis.
Articular processes centered around the odontoid have
smooth superior facets that facilitate rotational
articulation within the atlas. The inferior facets are
more posterior and in-line with the articular processes
of the rest of the cervical vertebrae area. On a lateral
view, the axis appears much like a typical cervical
vertebra, however, it is easily identified by the odontoid
process projecting vertically from the body and the large
and wide spinous process.
View odontoid view.
 On an open-mouth odontoid view, the axis is shaped
like a fat bowling pin with wings. The odontoid and the
body form the bowling pin, and the articular processes
are the wings.
The articulation of the odontoid and the atlantal
anterior arch is unique. Anteriorly, it is between the two
bones; posteriorly, the dens articulates with the
transverse ligament that is attached to the inner
aspects of the atlantal lateral masses. The spinal cord
travels in the space posterior to the transverse
ligament.
View C1-C2 cross section CT scan.
On an open-mouth odontoid view, the axis is shaped
like a fat bowling pin with wings. The odontoid and the
body form the bowling pin, and the articular processes
are the wings.
The articulation of the odontoid and the atlantal
anterior arch is unique. Anteriorly, it is between the two
bones; posteriorly, the dens articulates with the
transverse ligament that is attached to the inner
aspects of the atlantal lateral masses. The spinal cord
travels in the space posterior to the transverse
ligament.
View C1-C2 cross section CT scan.
 The upper image is a CT scan axial image through
the ring of C1. The odontoid process is visible
anteriorly in the ring. The transverse ligament is not
easily visible on this CT cut; however, it is posterior to
the odontoid. The spinal cord is visible in the posterior
portion of the ring of C1 (the spinal canal). Note the
fracture in the anterior aspect of C1. The gap in the
posterior portion of C1 is a growth plate. Compare this
CT image with the bony model of C1 and C2.
View open mouth odontoid view.
The upper image is a CT scan axial image through
the ring of C1. The odontoid process is visible
anteriorly in the ring. The transverse ligament is not
easily visible on this CT cut; however, it is posterior to
the odontoid. The spinal cord is visible in the posterior
portion of the ring of C1 (the spinal canal). Note the
fracture in the anterior aspect of C1. The gap in the
posterior portion of C1 is a growth plate. Compare this
CT image with the bony model of C1 and C2.
View open mouth odontoid view.
 Developmentally, the bodies of the axis and the
dens arise from separate ossification centers. The
odontoid (dens) itself has three ossification centers.
There are two columnar centers, forming the body of
the odontoid that typically fuse before birth, and a
third center at the tip of the odontoid. During infancy,
before the tip of the odontoid has ossified, the
superior end of the odontoid may have a cleft in it
radiographically. The odontoid of children may have a
separate ossification center at the tip of the
odontoid--the os terminale. A finding of a fragment at
the superior-most tip of the odontoid may be due to a
fracture or it may a normal ossification pattern.
The most common normal radiographic pattern
mistaken for an odontoid fracture is the subdental
synchondrosis. This is a linear lucency at the base of
the dens. The dens usually fuses with the body of C2
somewhere between ages 3 and 6 years. However, a
thin, sclerotic "scar" of the synchondrosis may be
appreciable on the lateral view for many years
thereafter.
Normal laxity of the soft tissues of the
cervicocranium in the developing pediatric patient can
make radiologic interpretations more difficult. Laxity of
the prevertebral tissues can resemble abscesses,
hematomas, or tumors, particularly if the film is taken in
exhalation or in flexion. Laxity of the transverse atlantal
ligaments -- spanning from the dens to the inner aspect
of the lateral masses of the atlas -- allow greater range
of motion between these two bones. This, in addition to
the cartilaginous (non-ossified) nature of the outer
layers of the odontoid, accounts for an increased
anterior atlanto-odontoid (atlantodental) interval of 3-5
mm in infants. In addition, the margins of the anterior
atlanto-odontoid interval can lose their parallelism
during neck flexion. These pediatric norms can
resemble atlantoaxial subluxation. Furthermore, laxity
of the ligamentous structures around C3 can also
resemble subluxation at the C2-C3 or C3-C4 junctions.
Radiographic Views
The three most common views employed in the
emergency department are: 1) the lateral view, 2) the
AP view, and 3) the AP open mouth odontoid. The
lateral view can be taken as a cross-table lateral while
the patient is still on a spine board in the emergency
department. The anteroposterior views often require
transporting the patient to the imaging department.
Below is an introduction to reading these three common
views.
Lateral neck
The lateral cervical spine radiograph is the most
useful view. As many as 80-90% of cervical spine
injuries can be detected on the lateral view alone. The
quality of the film image obtained should be assessed.
All cervical vertebrae, C1-C7, and the top part of T1
should ideally be visible. It is important to be able to
count all 7 cervical and one thoracic vertebrae since the
most common lesions occur at the upper and lower
ends of the cervical spine. The most commonly missed
lesions occur at the C7-T1 junction simply because it is
not shown on the film.
To assess C-spine alignment, four imaginary lines
can be drawn on the lateral film; which aid evaluation of
vertebral alignment: 1) anterior longitudinal line, 2)
posterior longitudinal line, 3) posterior facet margins
(not shown on diagram), and 4) spinolaminar line.
View lateral.
Developmentally, the bodies of the axis and the
dens arise from separate ossification centers. The
odontoid (dens) itself has three ossification centers.
There are two columnar centers, forming the body of
the odontoid that typically fuse before birth, and a
third center at the tip of the odontoid. During infancy,
before the tip of the odontoid has ossified, the
superior end of the odontoid may have a cleft in it
radiographically. The odontoid of children may have a
separate ossification center at the tip of the
odontoid--the os terminale. A finding of a fragment at
the superior-most tip of the odontoid may be due to a
fracture or it may a normal ossification pattern.
The most common normal radiographic pattern
mistaken for an odontoid fracture is the subdental
synchondrosis. This is a linear lucency at the base of
the dens. The dens usually fuses with the body of C2
somewhere between ages 3 and 6 years. However, a
thin, sclerotic "scar" of the synchondrosis may be
appreciable on the lateral view for many years
thereafter.
Normal laxity of the soft tissues of the
cervicocranium in the developing pediatric patient can
make radiologic interpretations more difficult. Laxity of
the prevertebral tissues can resemble abscesses,
hematomas, or tumors, particularly if the film is taken in
exhalation or in flexion. Laxity of the transverse atlantal
ligaments -- spanning from the dens to the inner aspect
of the lateral masses of the atlas -- allow greater range
of motion between these two bones. This, in addition to
the cartilaginous (non-ossified) nature of the outer
layers of the odontoid, accounts for an increased
anterior atlanto-odontoid (atlantodental) interval of 3-5
mm in infants. In addition, the margins of the anterior
atlanto-odontoid interval can lose their parallelism
during neck flexion. These pediatric norms can
resemble atlantoaxial subluxation. Furthermore, laxity
of the ligamentous structures around C3 can also
resemble subluxation at the C2-C3 or C3-C4 junctions.
Radiographic Views
The three most common views employed in the
emergency department are: 1) the lateral view, 2) the
AP view, and 3) the AP open mouth odontoid. The
lateral view can be taken as a cross-table lateral while
the patient is still on a spine board in the emergency
department. The anteroposterior views often require
transporting the patient to the imaging department.
Below is an introduction to reading these three common
views.
Lateral neck
The lateral cervical spine radiograph is the most
useful view. As many as 80-90% of cervical spine
injuries can be detected on the lateral view alone. The
quality of the film image obtained should be assessed.
All cervical vertebrae, C1-C7, and the top part of T1
should ideally be visible. It is important to be able to
count all 7 cervical and one thoracic vertebrae since the
most common lesions occur at the upper and lower
ends of the cervical spine. The most commonly missed
lesions occur at the C7-T1 junction simply because it is
not shown on the film.
To assess C-spine alignment, four imaginary lines
can be drawn on the lateral film; which aid evaluation of
vertebral alignment: 1) anterior longitudinal line, 2)
posterior longitudinal line, 3) posterior facet margins
(not shown on diagram), and 4) spinolaminar line.
View lateral.
 The anterior and posterior longitudinal lines simply
correspond to the locations of the anterior and posterior
longitudinal ligaments. The spinolaminar line
demarcates the posterior limits of the spinal canal.
These lordotic contours should be smooth and without
step-offs.
The neck is normally positioned with lordosis
(extension). In adults, a straight C-spine (lack of
lordosis) indicates the presence of muscle spasm and a
possible occult fracture. In children, the absence of
lordosis is commonly seen. When positioned on a
spine board, the large occiput of most children positions
their neck in a straight (without lordosis) or in a flexed
alignment. This is common and does not necessarily
indicate the presence of a significant injury. However, it
does make interpretation of the radiographs more
difficult since such poor positioning may cause
artifact radiographic abnormalities.
Proper positioning of the atlantoaxial bones with the
occiput can be assessed by noting the alignment of two
imaginary lines. First, extension of a line down the
slope of the clivus should point to the superior end of
the dens (the os terminale). The posterior margin of the
foramen magnum should be in line with the
spinolaminar line. Such an alignment places the
foramen magnum in-line with the spinal canal, this
corresponds to the junction of the brain stem and the
spinal cord.
Dislocation of articular facets or a fractured
vertebrae may result in a discontinuity of the contours
of these lines with implications of instability and
decreased patency of the spinal canal lumen resulting
in impingement of the spinal cord.
Widening of the retropharyngeal space is a sign of
injury to either soft tissue or the adjacent vertebrae.
The retropharyngeal space (essentially, the
pre-vertebral soft tissue space) should be roughly half
the width of a vertebral body. Fractures of the C-spine
can result in hemorrhaging into the retropharyngeal
space, resulting in widening of this soft tissue space on
the lateral neck view.
The spacing of the facet joints, intervertebral
spaces, and interspinous gaps can provide hints to the
integrity of the mechanical stability of the connections
between vertebrae. The width of these spaces should
be fairly constant between sequential vertebrae. The
articular surfaces should be parallel to each other. In
addition, the spinous processes are generally
equidistant from each other but converge toward a point
at the base of the posterior neck. Pathologically,
increased spacing often results from tearing of the
supporting ligaments. Increased interspinous
distances, "fanning," is often associated with a posterior
longitudinal ligament tear. Decreased spacing could
lead to invagination of connective tissue into the spinal
canal.
The major features of all vertebra should be
examined. The height of each vertebral body should be
fairly constant from C3 through T1. A slight decrease in
height of a vertebral body may be a compression
fracture. A difference of greater than 25% can occur
only if the posterior intervertebral ligaments are torn.
The pedicles, facets, and laminae of each vertebra
should be superimposed upon each other in a properly
taken radiograph. Doubling of facets and articular
columns should be examined for evidence of unilateral
or bilateral dislocated facets.
The cortical surfaces of each vertebra should be
scrutinized for steps, breaks, or abnormal angulations.
Blurred edges may result from fractures or dislocations.
Often the tendons and ligaments are stronger than the
bones themselves, and tear-drop shaped pieces of
bone could be avulsed by a strong force acting on the
anterior longitudinal ligament. In the clay shoveller's
fracture (spinous process fracture), a downward force
on the supraspinous ligament shears most of the C6 or
C7 spinous process off its base.
AP View
The AP view is helpful in evaluating the vertical
alignment of the spinous processes and the
visualization of the vertebral body from the AP
perspective. This view is also important in evaluating
lateral displacement of fractures or entire vertebrae.
View AP.
The anterior and posterior longitudinal lines simply
correspond to the locations of the anterior and posterior
longitudinal ligaments. The spinolaminar line
demarcates the posterior limits of the spinal canal.
These lordotic contours should be smooth and without
step-offs.
The neck is normally positioned with lordosis
(extension). In adults, a straight C-spine (lack of
lordosis) indicates the presence of muscle spasm and a
possible occult fracture. In children, the absence of
lordosis is commonly seen. When positioned on a
spine board, the large occiput of most children positions
their neck in a straight (without lordosis) or in a flexed
alignment. This is common and does not necessarily
indicate the presence of a significant injury. However, it
does make interpretation of the radiographs more
difficult since such poor positioning may cause
artifact radiographic abnormalities.
Proper positioning of the atlantoaxial bones with the
occiput can be assessed by noting the alignment of two
imaginary lines. First, extension of a line down the
slope of the clivus should point to the superior end of
the dens (the os terminale). The posterior margin of the
foramen magnum should be in line with the
spinolaminar line. Such an alignment places the
foramen magnum in-line with the spinal canal, this
corresponds to the junction of the brain stem and the
spinal cord.
Dislocation of articular facets or a fractured
vertebrae may result in a discontinuity of the contours
of these lines with implications of instability and
decreased patency of the spinal canal lumen resulting
in impingement of the spinal cord.
Widening of the retropharyngeal space is a sign of
injury to either soft tissue or the adjacent vertebrae.
The retropharyngeal space (essentially, the
pre-vertebral soft tissue space) should be roughly half
the width of a vertebral body. Fractures of the C-spine
can result in hemorrhaging into the retropharyngeal
space, resulting in widening of this soft tissue space on
the lateral neck view.
The spacing of the facet joints, intervertebral
spaces, and interspinous gaps can provide hints to the
integrity of the mechanical stability of the connections
between vertebrae. The width of these spaces should
be fairly constant between sequential vertebrae. The
articular surfaces should be parallel to each other. In
addition, the spinous processes are generally
equidistant from each other but converge toward a point
at the base of the posterior neck. Pathologically,
increased spacing often results from tearing of the
supporting ligaments. Increased interspinous
distances, "fanning," is often associated with a posterior
longitudinal ligament tear. Decreased spacing could
lead to invagination of connective tissue into the spinal
canal.
The major features of all vertebra should be
examined. The height of each vertebral body should be
fairly constant from C3 through T1. A slight decrease in
height of a vertebral body may be a compression
fracture. A difference of greater than 25% can occur
only if the posterior intervertebral ligaments are torn.
The pedicles, facets, and laminae of each vertebra
should be superimposed upon each other in a properly
taken radiograph. Doubling of facets and articular
columns should be examined for evidence of unilateral
or bilateral dislocated facets.
The cortical surfaces of each vertebra should be
scrutinized for steps, breaks, or abnormal angulations.
Blurred edges may result from fractures or dislocations.
Often the tendons and ligaments are stronger than the
bones themselves, and tear-drop shaped pieces of
bone could be avulsed by a strong force acting on the
anterior longitudinal ligament. In the clay shoveller's
fracture (spinous process fracture), a downward force
on the supraspinous ligament shears most of the C6 or
C7 spinous process off its base.
AP View
The AP view is helpful in evaluating the vertical
alignment of the spinous processes and the
visualization of the vertebral body from the AP
perspective. This view is also important in evaluating
lateral displacement of fractures or entire vertebrae.
View AP.
 Typically, in this view, the mandible and occiput are
superimposed over C1 and C2, and sometimes the
upper portions of C3 may be obscured. An adequate
film should clearly show the vertebral column from C3
to T1.
Spinous processes should be aligned in the midline
and be generally equidistant from one another.
Misalignment of the spinous processes may suggest a
dislocation or a fracture of an articular surface.
Increased spacing between spinous processes or an
apparent missing spinous process in this view may
suggest a fractured spinous process, as in the clay
shoveller's fracture (spinous process fracture). A
widened gap may also be due to a tear of the posterior
longitudinal ligament, resulting in "fanning" as seen on a
lateral radiograph.
The trachea is easily visualized in this view.
Disruption of tracheal radiolucency may also indicate
nearby lesions.
The intervertebral spaces should be evaluated for
uniformity from one vertebral pair to another. The
spaces should be of similar distances apart and the
articular surfaces should be fairly parallel to each other.
Dislocations and ligamentous tears may produce
widened or narrowed joint spaces in an AP view.
Lastly, the vertebrae should be evaluated for
fractures. The cortical surfaces should be continuous
and well defined. Each vertebral body should be
rectangular and of similar size. The uncinate
processes (U), bilateral raised lips on the superior
surface of the vertebral bodies, are most easily
evaluated for fractures from this AP view.
Open-Mouth Odontoid View
The AP open-mouth odontoid radiograph is used to
evaluate the cervicocranium from another perspective.
It is most valuable in assessing the relationship
between the lateral masses of the atlas and the axis.
The junction between C1 and C2 should be clearly
visible. Visibility of the entire odontoid process is of
secondary importance.
View odontoid view.
Typically, in this view, the mandible and occiput are
superimposed over C1 and C2, and sometimes the
upper portions of C3 may be obscured. An adequate
film should clearly show the vertebral column from C3
to T1.
Spinous processes should be aligned in the midline
and be generally equidistant from one another.
Misalignment of the spinous processes may suggest a
dislocation or a fracture of an articular surface.
Increased spacing between spinous processes or an
apparent missing spinous process in this view may
suggest a fractured spinous process, as in the clay
shoveller's fracture (spinous process fracture). A
widened gap may also be due to a tear of the posterior
longitudinal ligament, resulting in "fanning" as seen on a
lateral radiograph.
The trachea is easily visualized in this view.
Disruption of tracheal radiolucency may also indicate
nearby lesions.
The intervertebral spaces should be evaluated for
uniformity from one vertebral pair to another. The
spaces should be of similar distances apart and the
articular surfaces should be fairly parallel to each other.
Dislocations and ligamentous tears may produce
widened or narrowed joint spaces in an AP view.
Lastly, the vertebrae should be evaluated for
fractures. The cortical surfaces should be continuous
and well defined. Each vertebral body should be
rectangular and of similar size. The uncinate
processes (U), bilateral raised lips on the superior
surface of the vertebral bodies, are most easily
evaluated for fractures from this AP view.
Open-Mouth Odontoid View
The AP open-mouth odontoid radiograph is used to
evaluate the cervicocranium from another perspective.
It is most valuable in assessing the relationship
between the lateral masses of the atlas and the axis.
The junction between C1 and C2 should be clearly
visible. Visibility of the entire odontoid process is of
secondary importance.
View odontoid view.
 From this perspective, left and right symmetry is
most helpful in evaluation. The two atlantal lateral
masses should be equidistant from the dens, and the
articular surfaces of the atlantoaxial lateral masses
should be in perfect alignment. The inferior facets of
the atlantal (C1) lateral masses should be parallel to
and aligned with the upper facets of the axial (C2)
lateral masses (white arrows point to the lateral margin
of the facet joint). Lateral displacement of one or both
of the atlantal lateral masses (black arrow) is
suggestive of a Jefferson fracture in which the ring of
C1 is fractured, bursting it open displacing the lateral
masses outward.
The lateral masses should also be scrutinized for
unequal size. In rotary subluxation, the atlas is turned
such that one lateral mass is farther than the other from
the radiographic film and may appear larger. However,
rotary subluxation is best confirmed on a CT scan.
Laxity of ligamentous attachments surrounding the
odontoid and incomplete ossification of the odontoid
may allow up to two-thirds of the anterior atlantal arch
to be above the tip of the odontoid process.
Fractures of the odontoid are common and can be
seen on lateral and open-mouth odontoid views. These
fractures are classified according to the location of the
fracture. Type I is an oblique fracture through the upper
portion of the odontoid. It should be noted that
sometimes the upper incisors can obscure portions of
the upper odontoid and simulate a Type I fracture.
Type II fractures occur at the base of the odontoid
where it joins the body of C2. This is the most common
odontoid fracture. Unfortunately, this is also the
location of the subdental synchondrosis.
NOTE: While it is not unusual for the odontoid to be
tilted posteriorly, it should NOT be tilted anteriorly. This
is more indicative of an odontoid fracture. Widening of
the subdental synchondrosis coupled with anterior tilting
of the odontoid are highly indicative of an odontoid
fracture.
A Type III odontoid fracture extends into the
vertebral body of C2.
The odontoid image shows three open mouth
odontoid radiographs on the right. The upper
radiograph shows the odontoid well. However, the
lateral margins of the lateral masses of C1 and C2 are
obscured by the patient's lower teeth, making it
impossible to assess the lateral alignment of the C1-C2
facet joints.
The middle image shows a bursting ring fracture of
C1 with outward displacement of the C1 lateral masses
(black arrow). The lower image shows normal
alignment of the C1-C2 facet joints. The white arrow
points to the lateral margin of the facet joint.
Other Special Views
In addition to the standard three views (lateral, AP,
odontoid), other radiographic views can aid in obtaining
a better perspective on a suspected lesion.
Swimmer's View: Recall that an adequate lateral
film should reveal all seven cervical vertebrae and
upper T1. Typically, downward traction on the arms will
produce the adequate visualization in most cases.
Should the C7/T1 junction still be obscured, a
swimmer's view can be obtained by elevating the arm
closest to the film. This posture yields a slightly oblique
view of the vertebral column, but moves the shoulder
joint above the C7/T1 junction. C7/T1 can easily be
seen in this view; however, it is often overlapping with
dense soft tissue and the bones of the shoulder.
View swimmer's view.
From this perspective, left and right symmetry is
most helpful in evaluation. The two atlantal lateral
masses should be equidistant from the dens, and the
articular surfaces of the atlantoaxial lateral masses
should be in perfect alignment. The inferior facets of
the atlantal (C1) lateral masses should be parallel to
and aligned with the upper facets of the axial (C2)
lateral masses (white arrows point to the lateral margin
of the facet joint). Lateral displacement of one or both
of the atlantal lateral masses (black arrow) is
suggestive of a Jefferson fracture in which the ring of
C1 is fractured, bursting it open displacing the lateral
masses outward.
The lateral masses should also be scrutinized for
unequal size. In rotary subluxation, the atlas is turned
such that one lateral mass is farther than the other from
the radiographic film and may appear larger. However,
rotary subluxation is best confirmed on a CT scan.
Laxity of ligamentous attachments surrounding the
odontoid and incomplete ossification of the odontoid
may allow up to two-thirds of the anterior atlantal arch
to be above the tip of the odontoid process.
Fractures of the odontoid are common and can be
seen on lateral and open-mouth odontoid views. These
fractures are classified according to the location of the
fracture. Type I is an oblique fracture through the upper
portion of the odontoid. It should be noted that
sometimes the upper incisors can obscure portions of
the upper odontoid and simulate a Type I fracture.
Type II fractures occur at the base of the odontoid
where it joins the body of C2. This is the most common
odontoid fracture. Unfortunately, this is also the
location of the subdental synchondrosis.
NOTE: While it is not unusual for the odontoid to be
tilted posteriorly, it should NOT be tilted anteriorly. This
is more indicative of an odontoid fracture. Widening of
the subdental synchondrosis coupled with anterior tilting
of the odontoid are highly indicative of an odontoid
fracture.
A Type III odontoid fracture extends into the
vertebral body of C2.
The odontoid image shows three open mouth
odontoid radiographs on the right. The upper
radiograph shows the odontoid well. However, the
lateral margins of the lateral masses of C1 and C2 are
obscured by the patient's lower teeth, making it
impossible to assess the lateral alignment of the C1-C2
facet joints.
The middle image shows a bursting ring fracture of
C1 with outward displacement of the C1 lateral masses
(black arrow). The lower image shows normal
alignment of the C1-C2 facet joints. The white arrow
points to the lateral margin of the facet joint.
Other Special Views
In addition to the standard three views (lateral, AP,
odontoid), other radiographic views can aid in obtaining
a better perspective on a suspected lesion.
Swimmer's View: Recall that an adequate lateral
film should reveal all seven cervical vertebrae and
upper T1. Typically, downward traction on the arms will
produce the adequate visualization in most cases.
Should the C7/T1 junction still be obscured, a
swimmer's view can be obtained by elevating the arm
closest to the film. This posture yields a slightly oblique
view of the vertebral column, but moves the shoulder
joint above the C7/T1 junction. C7/T1 can easily be
seen in this view; however, it is often overlapping with
dense soft tissue and the bones of the shoulder.
View swimmer's view.
 In this swimmer's view, note that the lower cervical
spine can be seen, but in this case, it is still not optimal
since C7 is still not visualized.
Oblique Projections: The oblique views provide
good visualization of the posterior structures of the
vertebral column, such as the intervertebral foramina
and articulation of the facets. They are particularly
helpful in evaluating suspected unilateral facet
dislocations since only one half of the facets and
intervertebral foramina are viewed at a time. The
foramina are also best visualized on these views.
View oblique views.
In this swimmer's view, note that the lower cervical
spine can be seen, but in this case, it is still not optimal
since C7 is still not visualized.
Oblique Projections: The oblique views provide
good visualization of the posterior structures of the
vertebral column, such as the intervertebral foramina
and articulation of the facets. They are particularly
helpful in evaluating suspected unilateral facet
dislocations since only one half of the facets and
intervertebral foramina are viewed at a time. The
foramina are also best visualized on these views.
View oblique views.
 Lateral Flexion and Extension Views: The flexion
and extension views are obtained on a conscious
patient who can actively bend their neck. Care must be
taken in obtaining these views as there is risk of further
displacement. In appropriate circumstances, these
views may be particularly helpful in excluding
ligamentous injury and potential instability. Some
physicians have found the flexion view invaluable in
detecting occult posterior ligamentous injuries resulting
from hyperflexion.
References
1. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - I. BMJ
Sept1993;307(25):785-789.
2. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - II. BMJ
Oct1993:307(2):855-859.
3. Ellis GL. Imaging of the Atlas (C1) and Axis
(C2). Emergency Medicine Clinics of North America.
1991;9(4):719-731.
4. Gerlock AJ, et al. Advanced Excercises in
Diagnositic Radiology - 11: The Cervical Spine in
Trauma. Philadelphia, W. B. Saunders Company,
1978.
5. Goldberg S. Clinical Anatomy made Ridiculously
Simple. Miami, MedMaster, Inc. 1986.
6. Harris JH, Mirvis SE. The Radiology of Acute
Cervical Spine Trauma, Third Edition. Baltimore,
Williams & Wilkins, 1996, pp.1-72, 86, 180-196.
7. Montgomery JL, Montgomery ML. Radiographic
evaluation ofcervical spine trauma: Procedures to avoid
catastrophe. Postgrad Med 1994;95(4):173-196.
8. Moore KL. Clinically Oriented Anatomy, Second
Edition. Baltimore, Williams & Wilkins, 1985, pp.
576-578, 585-596.
9. Netter FH. Atlas of Human Anatomy. Summit:
Ciba-GeigyCorporation, 1989. Plates 12-16, 30, 57, 59,
172.
10. Swisschuk LE. Emergency Imaging of The
Acutely Ill or Injured Child, Third Edition. Baltimore,
Williams & Wilkins, 1994, pp.653-717.
11. Walsh-Kelly CM, et al. Clinical impact of
radiograph misinterpretation in a pediatric ED and the
effect of physician training level. Am J Emerg Med
1995;13(3): 262-264.
12. Harris JH, Harris WH, Novelline RA. The
Radiology of Emergency Medicine, third edition.
Baltimore, Williams & WIlkins, 1993, pp. 127-244.
Lateral Flexion and Extension Views: The flexion
and extension views are obtained on a conscious
patient who can actively bend their neck. Care must be
taken in obtaining these views as there is risk of further
displacement. In appropriate circumstances, these
views may be particularly helpful in excluding
ligamentous injury and potential instability. Some
physicians have found the flexion view invaluable in
detecting occult posterior ligamentous injuries resulting
from hyperflexion.
References
1. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - I. BMJ
Sept1993;307(25):785-789.
2. Driscoll PA, Ross R, Nicholson DA. ABC of
Emergency Radiology: Cervical Spine - II. BMJ
Oct1993:307(2):855-859.
3. Ellis GL. Imaging of the Atlas (C1) and Axis
(C2). Emergency Medicine Clinics of North America.
1991;9(4):719-731.
4. Gerlock AJ, et al. Advanced Excercises in
Diagnositic Radiology - 11: The Cervical Spine in
Trauma. Philadelphia, W. B. Saunders Company,
1978.
5. Goldberg S. Clinical Anatomy made Ridiculously
Simple. Miami, MedMaster, Inc. 1986.
6. Harris JH, Mirvis SE. The Radiology of Acute
Cervical Spine Trauma, Third Edition. Baltimore,
Williams & Wilkins, 1996, pp.1-72, 86, 180-196.
7. Montgomery JL, Montgomery ML. Radiographic
evaluation ofcervical spine trauma: Procedures to avoid
catastrophe. Postgrad Med 1994;95(4):173-196.
8. Moore KL. Clinically Oriented Anatomy, Second
Edition. Baltimore, Williams & Wilkins, 1985, pp.
576-578, 585-596.
9. Netter FH. Atlas of Human Anatomy. Summit:
Ciba-GeigyCorporation, 1989. Plates 12-16, 30, 57, 59,
172.
10. Swisschuk LE. Emergency Imaging of The
Acutely Ill or Injured Child, Third Edition. Baltimore,
Williams & Wilkins, 1994, pp.653-717.
11. Walsh-Kelly CM, et al. Clinical impact of
radiograph misinterpretation in a pediatric ED and the
effect of physician training level. Am J Emerg Med
1995;13(3): 262-264.
12. Harris JH, Harris WH, Novelline RA. The
Radiology of Emergency Medicine, third edition.
Baltimore, Williams & WIlkins, 1993, pp. 127-244.