Right Lower Quadrant Pain in a 13-Year Old Female
Radiology Cases in Pediatric Emergency Medicine
Volume 4, Case 8
Brunhild Halm, M.D.
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a 13 year old female who presents to the
E.D. with a one day history of increasing intermittent
RLQ pain and the complaint of feeling "full". She
describes the pain as sharp and stabbing without
radiation. Standing, running, and deep breathing make
it worse. There is no history of vomiting, diarrhea, or
fever. She denies urgency, frequency, or burning on
urination. She has had similar pain of less severity for
the last two years, especially when running. She has
never had a menstrual period and denies being sexually
active.
She was born in Vietnam and moved to the U.S. two
years ago. Her PMH is negative. Medications: None.
Immunizations are UTD.
Exam: VS T 38.8, P 118, R 24, BP 108/69. She is
awake, alert, cooperative, and in no distress. Oral
mucosa moist. Heart regular, no murmurs. Lungs
clear. Abdomen non-distended. There is mild to
moderate tenderness in both lower quadrants and in the
suprapubic area, but no rebound tenderness or
guarding. There are no palpable masses. Bowel
sounds are active. Tanner Stage: Breasts IV, Pubic
hair IV. Color and perfusion are good. Extremities
unremarkable.
Laboratory studies:
CBC WBC 15,500, 76% segs, 12% bands, 3%
lymphs, 9% monos. Hgb 12.8, Hct 39.1. Platelet count
265,000. Chemistry panel normal. Urinalysis normal.
Urine HCG negative.
What is your diagnosis at this point?
An adolescent female presents with a long-standing
history of intermittent abdominal pain that acutely
worsens. She has well-developed secondary sex
characteristics but has not reached menarche. This
makes an obstruction of the genital tract likely.
Obstruction of the genital tract results in the
accumulation of secretions, blood, or both within the
uterus, vagina, or both, depending on the level of
obstruction. The three main types of congenital vaginal
obstructions are:
1. Segmental atresia, usually midvagina.
2. Transverse vaginal septum, most common in the
midportion.
3. Imperforate hymen.
View diagram of these types.
 The vagina proximally, and often the uterus are
dilated, resulting in hydro(metro)colpos at birth or
hemato(metro)colpos at puberty. Examination of the
genitalia in our patient reveals a thick, tense, bulging
hymen at the introitus, which establishes the diagnosis
of imperforate hymen. On rectal exam a midline mass
is palpable anteriorly.
A pelvic ultrasound is performed.
View pelvic ultrasound.
The vagina proximally, and often the uterus are
dilated, resulting in hydro(metro)colpos at birth or
hemato(metro)colpos at puberty. Examination of the
genitalia in our patient reveals a thick, tense, bulging
hymen at the introitus, which establishes the diagnosis
of imperforate hymen. On rectal exam a midline mass
is palpable anteriorly.
A pelvic ultrasound is performed.
View pelvic ultrasound.
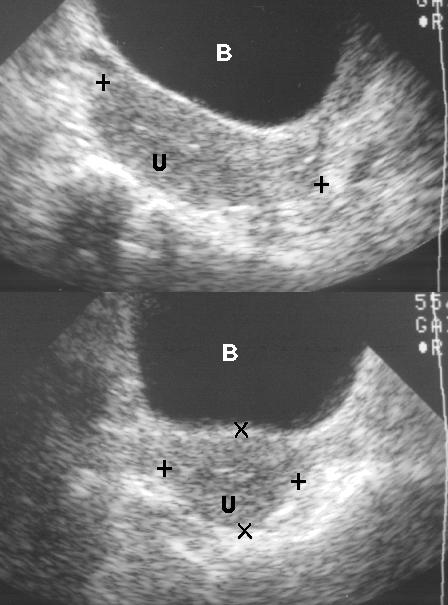
 The sagittal view or long axis of the uterus (shown
above) and transverse view (shown below) shows
marked distention of the endometrial cavity,
compressing the bladder anteriorly. Scattered internal
echoes represent blood, and mucous debris. The uterus
is enlarged (14.9 cm by 8.3 cm by 6.3 cm).
View labeling on ultrasound.
The sagittal view or long axis of the uterus (shown
above) and transverse view (shown below) shows
marked distention of the endometrial cavity,
compressing the bladder anteriorly. Scattered internal
echoes represent blood, and mucous debris. The uterus
is enlarged (14.9 cm by 8.3 cm by 6.3 cm).
View labeling on ultrasound.
 The uterine cavity is labeled as "U". The bladder
(labeled "B") is compressed. The anterior abdominal
wall musculature is labeled as "M". The crosses mark
the boundaries of the uterus.
Contrast this with an ultrasound of the normal post
pubertal uterus.
View normal pelvic ultrasound.
The uterine cavity is labeled as "U". The bladder
(labeled "B") is compressed. The anterior abdominal
wall musculature is labeled as "M". The crosses mark
the boundaries of the uterus.
Contrast this with an ultrasound of the normal post
pubertal uterus.
View normal pelvic ultrasound.
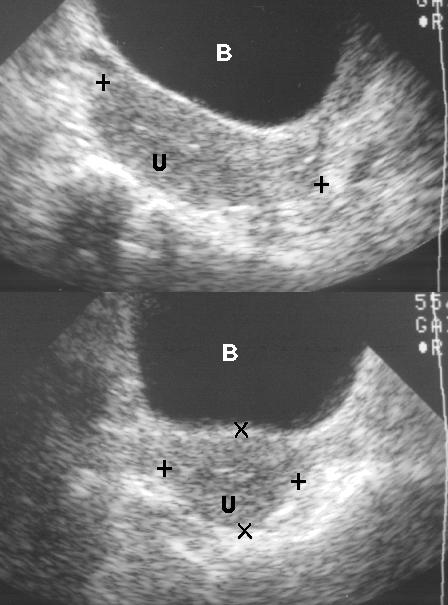
 The sagittal view is shown above. The transverse
view is shown below. The maximum dimensions of the
nulliparous uterus are approximately 8cm in length by
5cm in width by 4cm in AP diameter. The normal
endometrial cavity is seen as a thin echogenic line as a
result of reflection from the interface between the
opposing surfaces of the endometrium.
View labeling on this normal ultrasound.
The sagittal view is shown above. The transverse
view is shown below. The maximum dimensions of the
nulliparous uterus are approximately 8cm in length by
5cm in width by 4cm in AP diameter. The normal
endometrial cavity is seen as a thin echogenic line as a
result of reflection from the interface between the
opposing surfaces of the endometrium.
View labeling on this normal ultrasound.
 The bladder (labeled "B") is dilated and fluid-filled in
both views to optimize the transmission of ultrasound
from the anterior pelvis. The sagittal view (above)
shows the myometrial wall labeled as "U". The thin
echogenic (white) line above the "U" represents the
endometrial cavity with the opposing myometrium
above this. In the transverse view (below), the
myometrium is labeled as "U". The echogenic
endometrial cavity is just above the letter "U" with the
opposing myometrial wall above this. The crosses
mark the outer dimensions of the uterus in both views.
Our patient is taken to the operating room. A
hymenectomy is performed, which allows the
accumulated menstrual blood and vaginal secretions to
drain.
An imperforate hymen is a rare lesion, but it is the
most common truly obstructive abnormality of the
genital tract. In one survey, it occurred in 0.1% of full
term female neonates. In imperforate hymen, the
vagina is obliterated by a thick membrane interpreted
as hymen, since no hymen remnants are identified.
Some patients may present at birth with a large midline
mass due to accumulation of vaginal secretions
secondary to stimulation by maternal hormones. The
uterus and fallopian tubes may also be dilated
(hydrometrocolpos). In the presence of neonatal
withdrawal bleed, a hematocolpos may develop, which
presents as a dark purplish bulge at the introitus. Most
patients are asymptomatic at birth and during
childhood, but present in late puberty with primary
amenorrhea, cyclical crampy abdominal pain, and a
pelvic mass due to accumulation of menstrual blood.
An imperforate hymen is not of Mullerian origin;
therefore it is not associated with other genitourinary
abnormalities. However, hematocolpos or hydrocolpos
may lead to complete urethral obstruction or variable
degrees of hydroureter or hydronephrosis as a result of
the chronic extrinsic pressure. Patients with
imperforate hymen associated with hematocolpos also
have an increased risk of endometriosis, which is felt to
be secondary to the mechanical obstruction and
metaplasia. If this retrograde flow is stopped early
enough, endometriosis might be prevented. Therefore,
surgery should be scheduled promptly for adolescents,
but can be delayed and performed electively for
asymptomatic infants and children.
References:
1. Paradise JE. Pediatric and Adolescent
Gynecology. In: Fleisher GR, Ludwig S. Textbook of
Pediatric Emergency Medicine, 3rd edition. Baltimore,
Williams and Wilkins, 1993, pp. 916-919.
2. Salem S. The Uterus and Adnexa. In: Rumack
CM,Wilson SR, Charboneau JW. Diagnostic
Ultrasound, Volume 1. St. Louis, 1991, pp. 384-387.
3. Currarino G, Wood B, Majd M. The Genitourinary
Tract and Retroperitoneum. In: Silverman FN, Kuhn
JP. Caffey's Pediatric X-Ray Diagnosis, Ninth edition,
Volume 2. St. Louis, 1993, pp. 1384-1388.
4. Sanfilippo J. Endometriosis in association with
uterine anomaly. American Journal of Obstetrics and
Gynecology, 1986;154: 39-43.
The bladder (labeled "B") is dilated and fluid-filled in
both views to optimize the transmission of ultrasound
from the anterior pelvis. The sagittal view (above)
shows the myometrial wall labeled as "U". The thin
echogenic (white) line above the "U" represents the
endometrial cavity with the opposing myometrium
above this. In the transverse view (below), the
myometrium is labeled as "U". The echogenic
endometrial cavity is just above the letter "U" with the
opposing myometrial wall above this. The crosses
mark the outer dimensions of the uterus in both views.
Our patient is taken to the operating room. A
hymenectomy is performed, which allows the
accumulated menstrual blood and vaginal secretions to
drain.
An imperforate hymen is a rare lesion, but it is the
most common truly obstructive abnormality of the
genital tract. In one survey, it occurred in 0.1% of full
term female neonates. In imperforate hymen, the
vagina is obliterated by a thick membrane interpreted
as hymen, since no hymen remnants are identified.
Some patients may present at birth with a large midline
mass due to accumulation of vaginal secretions
secondary to stimulation by maternal hormones. The
uterus and fallopian tubes may also be dilated
(hydrometrocolpos). In the presence of neonatal
withdrawal bleed, a hematocolpos may develop, which
presents as a dark purplish bulge at the introitus. Most
patients are asymptomatic at birth and during
childhood, but present in late puberty with primary
amenorrhea, cyclical crampy abdominal pain, and a
pelvic mass due to accumulation of menstrual blood.
An imperforate hymen is not of Mullerian origin;
therefore it is not associated with other genitourinary
abnormalities. However, hematocolpos or hydrocolpos
may lead to complete urethral obstruction or variable
degrees of hydroureter or hydronephrosis as a result of
the chronic extrinsic pressure. Patients with
imperforate hymen associated with hematocolpos also
have an increased risk of endometriosis, which is felt to
be secondary to the mechanical obstruction and
metaplasia. If this retrograde flow is stopped early
enough, endometriosis might be prevented. Therefore,
surgery should be scheduled promptly for adolescents,
but can be delayed and performed electively for
asymptomatic infants and children.
References:
1. Paradise JE. Pediatric and Adolescent
Gynecology. In: Fleisher GR, Ludwig S. Textbook of
Pediatric Emergency Medicine, 3rd edition. Baltimore,
Williams and Wilkins, 1993, pp. 916-919.
2. Salem S. The Uterus and Adnexa. In: Rumack
CM,Wilson SR, Charboneau JW. Diagnostic
Ultrasound, Volume 1. St. Louis, 1991, pp. 384-387.
3. Currarino G, Wood B, Majd M. The Genitourinary
Tract and Retroperitoneum. In: Silverman FN, Kuhn
JP. Caffey's Pediatric X-Ray Diagnosis, Ninth edition,
Volume 2. St. Louis, 1993, pp. 1384-1388.
4. Sanfilippo J. Endometriosis in association with
uterine anomaly. American Journal of Obstetrics and
Gynecology, 1986;154: 39-43.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 The vagina proximally, and often the uterus are
dilated, resulting in hydro(metro)colpos at birth or
hemato(metro)colpos at puberty. Examination of the
genitalia in our patient reveals a thick, tense, bulging
hymen at the introitus, which establishes the diagnosis
of imperforate hymen. On rectal exam a midline mass
is palpable anteriorly.
A pelvic ultrasound is performed.
View pelvic ultrasound.
The vagina proximally, and often the uterus are
dilated, resulting in hydro(metro)colpos at birth or
hemato(metro)colpos at puberty. Examination of the
genitalia in our patient reveals a thick, tense, bulging
hymen at the introitus, which establishes the diagnosis
of imperforate hymen. On rectal exam a midline mass
is palpable anteriorly.
A pelvic ultrasound is performed.
View pelvic ultrasound.
 The sagittal view or long axis of the uterus (shown
above) and transverse view (shown below) shows
marked distention of the endometrial cavity,
compressing the bladder anteriorly. Scattered internal
echoes represent blood, and mucous debris. The uterus
is enlarged (14.9 cm by 8.3 cm by 6.3 cm).
View labeling on ultrasound.
The sagittal view or long axis of the uterus (shown
above) and transverse view (shown below) shows
marked distention of the endometrial cavity,
compressing the bladder anteriorly. Scattered internal
echoes represent blood, and mucous debris. The uterus
is enlarged (14.9 cm by 8.3 cm by 6.3 cm).
View labeling on ultrasound.
 The uterine cavity is labeled as "U". The bladder
(labeled "B") is compressed. The anterior abdominal
wall musculature is labeled as "M". The crosses mark
the boundaries of the uterus.
Contrast this with an ultrasound of the normal post
pubertal uterus.
View normal pelvic ultrasound.
The uterine cavity is labeled as "U". The bladder
(labeled "B") is compressed. The anterior abdominal
wall musculature is labeled as "M". The crosses mark
the boundaries of the uterus.
Contrast this with an ultrasound of the normal post
pubertal uterus.
View normal pelvic ultrasound.
 The sagittal view is shown above. The transverse
view is shown below. The maximum dimensions of the
nulliparous uterus are approximately 8cm in length by
5cm in width by 4cm in AP diameter. The normal
endometrial cavity is seen as a thin echogenic line as a
result of reflection from the interface between the
opposing surfaces of the endometrium.
View labeling on this normal ultrasound.
The sagittal view is shown above. The transverse
view is shown below. The maximum dimensions of the
nulliparous uterus are approximately 8cm in length by
5cm in width by 4cm in AP diameter. The normal
endometrial cavity is seen as a thin echogenic line as a
result of reflection from the interface between the
opposing surfaces of the endometrium.
View labeling on this normal ultrasound.
 The bladder (labeled "B") is dilated and fluid-filled in
both views to optimize the transmission of ultrasound
from the anterior pelvis. The sagittal view (above)
shows the myometrial wall labeled as "U". The thin
echogenic (white) line above the "U" represents the
endometrial cavity with the opposing myometrium
above this. In the transverse view (below), the
myometrium is labeled as "U". The echogenic
endometrial cavity is just above the letter "U" with the
opposing myometrial wall above this. The crosses
mark the outer dimensions of the uterus in both views.
Our patient is taken to the operating room. A
hymenectomy is performed, which allows the
accumulated menstrual blood and vaginal secretions to
drain.
An imperforate hymen is a rare lesion, but it is the
most common truly obstructive abnormality of the
genital tract. In one survey, it occurred in 0.1% of full
term female neonates. In imperforate hymen, the
vagina is obliterated by a thick membrane interpreted
as hymen, since no hymen remnants are identified.
Some patients may present at birth with a large midline
mass due to accumulation of vaginal secretions
secondary to stimulation by maternal hormones. The
uterus and fallopian tubes may also be dilated
(hydrometrocolpos). In the presence of neonatal
withdrawal bleed, a hematocolpos may develop, which
presents as a dark purplish bulge at the introitus. Most
patients are asymptomatic at birth and during
childhood, but present in late puberty with primary
amenorrhea, cyclical crampy abdominal pain, and a
pelvic mass due to accumulation of menstrual blood.
An imperforate hymen is not of Mullerian origin;
therefore it is not associated with other genitourinary
abnormalities. However, hematocolpos or hydrocolpos
may lead to complete urethral obstruction or variable
degrees of hydroureter or hydronephrosis as a result of
the chronic extrinsic pressure. Patients with
imperforate hymen associated with hematocolpos also
have an increased risk of endometriosis, which is felt to
be secondary to the mechanical obstruction and
metaplasia. If this retrograde flow is stopped early
enough, endometriosis might be prevented. Therefore,
surgery should be scheduled promptly for adolescents,
but can be delayed and performed electively for
asymptomatic infants and children.
References:
1. Paradise JE. Pediatric and Adolescent
Gynecology. In: Fleisher GR, Ludwig S. Textbook of
Pediatric Emergency Medicine, 3rd edition. Baltimore,
Williams and Wilkins, 1993, pp. 916-919.
2. Salem S. The Uterus and Adnexa. In: Rumack
CM,Wilson SR, Charboneau JW. Diagnostic
Ultrasound, Volume 1. St. Louis, 1991, pp. 384-387.
3. Currarino G, Wood B, Majd M. The Genitourinary
Tract and Retroperitoneum. In: Silverman FN, Kuhn
JP. Caffey's Pediatric X-Ray Diagnosis, Ninth edition,
Volume 2. St. Louis, 1993, pp. 1384-1388.
4. Sanfilippo J. Endometriosis in association with
uterine anomaly. American Journal of Obstetrics and
Gynecology, 1986;154: 39-43.
The bladder (labeled "B") is dilated and fluid-filled in
both views to optimize the transmission of ultrasound
from the anterior pelvis. The sagittal view (above)
shows the myometrial wall labeled as "U". The thin
echogenic (white) line above the "U" represents the
endometrial cavity with the opposing myometrium
above this. In the transverse view (below), the
myometrium is labeled as "U". The echogenic
endometrial cavity is just above the letter "U" with the
opposing myometrial wall above this. The crosses
mark the outer dimensions of the uterus in both views.
Our patient is taken to the operating room. A
hymenectomy is performed, which allows the
accumulated menstrual blood and vaginal secretions to
drain.
An imperforate hymen is a rare lesion, but it is the
most common truly obstructive abnormality of the
genital tract. In one survey, it occurred in 0.1% of full
term female neonates. In imperforate hymen, the
vagina is obliterated by a thick membrane interpreted
as hymen, since no hymen remnants are identified.
Some patients may present at birth with a large midline
mass due to accumulation of vaginal secretions
secondary to stimulation by maternal hormones. The
uterus and fallopian tubes may also be dilated
(hydrometrocolpos). In the presence of neonatal
withdrawal bleed, a hematocolpos may develop, which
presents as a dark purplish bulge at the introitus. Most
patients are asymptomatic at birth and during
childhood, but present in late puberty with primary
amenorrhea, cyclical crampy abdominal pain, and a
pelvic mass due to accumulation of menstrual blood.
An imperforate hymen is not of Mullerian origin;
therefore it is not associated with other genitourinary
abnormalities. However, hematocolpos or hydrocolpos
may lead to complete urethral obstruction or variable
degrees of hydroureter or hydronephrosis as a result of
the chronic extrinsic pressure. Patients with
imperforate hymen associated with hematocolpos also
have an increased risk of endometriosis, which is felt to
be secondary to the mechanical obstruction and
metaplasia. If this retrograde flow is stopped early
enough, endometriosis might be prevented. Therefore,
surgery should be scheduled promptly for adolescents,
but can be delayed and performed electively for
asymptomatic infants and children.
References:
1. Paradise JE. Pediatric and Adolescent
Gynecology. In: Fleisher GR, Ludwig S. Textbook of
Pediatric Emergency Medicine, 3rd edition. Baltimore,
Williams and Wilkins, 1993, pp. 916-919.
2. Salem S. The Uterus and Adnexa. In: Rumack
CM,Wilson SR, Charboneau JW. Diagnostic
Ultrasound, Volume 1. St. Louis, 1991, pp. 384-387.
3. Currarino G, Wood B, Majd M. The Genitourinary
Tract and Retroperitoneum. In: Silverman FN, Kuhn
JP. Caffey's Pediatric X-Ray Diagnosis, Ninth edition,
Volume 2. St. Louis, 1993, pp. 1384-1388.
4. Sanfilippo J. Endometriosis in association with
uterine anomaly. American Journal of Obstetrics and
Gynecology, 1986;154: 39-43.