Test Your Skill In Reading Pediatric Chest Radiographs
Radiology Cases in Pediatric Emergency Medicine
Volume 3, Case 20
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
Test your skill in reading these 16 pediatric chest
radiographs. Many of these have subtle findings.
Unfortunately, subtle findings become even less
obvious when they are displayed on a computer
monitor. They are reproduced here as best as
possible. You may need to darken the room lights and
adjust the contrast and brightness on your monitor to
appreciate some findings.
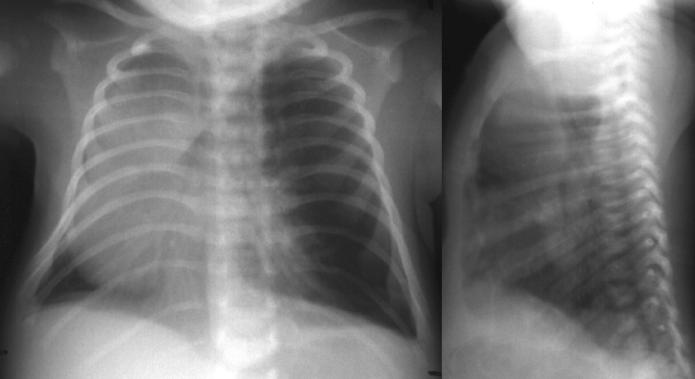
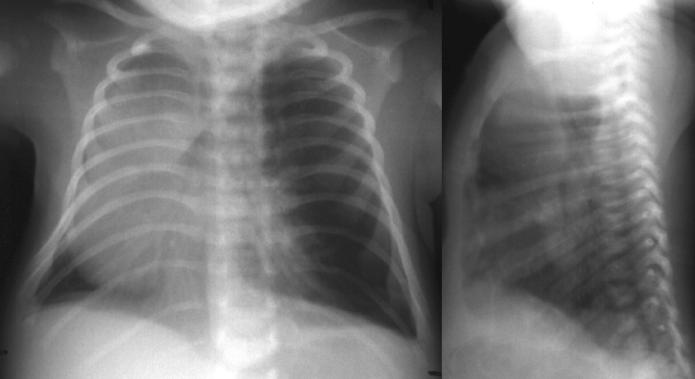
Case A:
This is a 15-month old male with fever, coughing,
and tachypnea.
View Case A.
 Interpretation of Case A
Bilateral central pulmonary infiltrates, but most
marked in the right middle and left lower lobes. The
left lower lobe infiltrate is best seen on the lateral
view inferiorly over the spine. The lungs are
hyperaerated.
Impression: Right middle and left lower lobe
infiltrates.
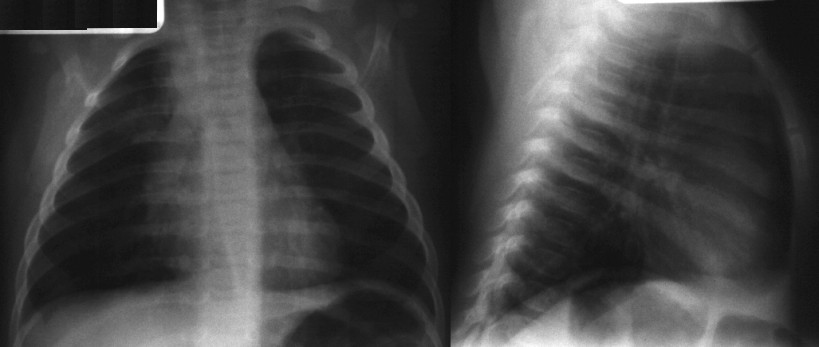
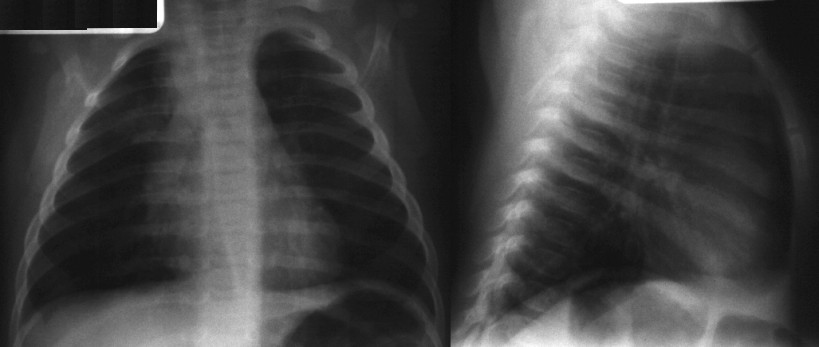
Case B:
This is a 3 year old female whose parents do not
speak English well. Her chief complaint is coughing
and difficulty breathing. There is mild bilateral stridor on
exam. Her cough sounds slightly bronchospastic, but
not barking in nature.
View Case B.
Interpretation of Case A
Bilateral central pulmonary infiltrates, but most
marked in the right middle and left lower lobes. The
left lower lobe infiltrate is best seen on the lateral
view inferiorly over the spine. The lungs are
hyperaerated.
Impression: Right middle and left lower lobe
infiltrates.
Case B:
This is a 3 year old female whose parents do not
speak English well. Her chief complaint is coughing
and difficulty breathing. There is mild bilateral stridor on
exam. Her cough sounds slightly bronchospastic, but
not barking in nature.
View Case B.
 Interpretation of Case B
No infiltrates are noted. The right side is more
lucent (darker) compared to the left. This is subtle and
may be difficult to appreciate unless you step back and
view the CXR from a distance. The right
hemidiaphragm is slightly higher than the left
hemidiaphragm, however, it should be higher than this.
Both these findings suggest right sided hyperexpansion.
More clinical history through a translator indicated that
she was jumping on a bed while eating some food
(thought to be meat), when she began choking. Since
that time, she has experienced respiratory difficulty.
Further radiographs revealed bilateral air trapping.
Bronchoscopy revealed bilateral bronchial peanut
fragment foreign bodies.
Impression: Right sided hyperexpansion and air
trapping. Possible bronchial foreign body.
Case C:
This is a two week old male infant who arrived in the
E.D. with a history of noisy breathing and worsening
respiratory distress. VS T36.7, P160, R60, BP 100/70.
His color is dusky. His oxygen saturation is 86% in
room air. Oxygen is applied and his color improves.
His oxygen saturation is now 96%. He has diminished
breath sounds bilaterally. There are moderately severe
retractions.
View Case C
Interpretation of Case B
No infiltrates are noted. The right side is more
lucent (darker) compared to the left. This is subtle and
may be difficult to appreciate unless you step back and
view the CXR from a distance. The right
hemidiaphragm is slightly higher than the left
hemidiaphragm, however, it should be higher than this.
Both these findings suggest right sided hyperexpansion.
More clinical history through a translator indicated that
she was jumping on a bed while eating some food
(thought to be meat), when she began choking. Since
that time, she has experienced respiratory difficulty.
Further radiographs revealed bilateral air trapping.
Bronchoscopy revealed bilateral bronchial peanut
fragment foreign bodies.
Impression: Right sided hyperexpansion and air
trapping. Possible bronchial foreign body.
Case C:
This is a two week old male infant who arrived in the
E.D. with a history of noisy breathing and worsening
respiratory distress. VS T36.7, P160, R60, BP 100/70.
His color is dusky. His oxygen saturation is 86% in
room air. Oxygen is applied and his color improves.
His oxygen saturation is now 96%. He has diminished
breath sounds bilaterally. There are moderately severe
retractions.
View Case C
 Interpretation of Case C
There is hyperlucency of the left chest with a
mediastinal and cardiac shift to the right. Although this
may look like a tension pneumothorax, realize that such
a large tension pneumothorax would generally be
associated with hypotension, bradycardia, and
persistent hypoxia (despite supplemental oxygen).
Since this infant appears to have good cardiovascular
function and his oxygenation improved with
supplemental oxygen, one should not immediately jump
to evacuating the left chest since he is currently stable.
After carefully reassessing the situation and
reexamining the CXR, it is evident that lung markings
are present in the left chest. This represents a
hyperexpanded lobe. The hyperexpansion is so severe
that it compresses the remaining left lung and pushes
the heart and mediastinum to the right, compressing the
right lung as well.
Impression: Left upper lobe hyperexpansion with
mediastinal shift. Congenital lobar emphysema. This
case is discussed in more detail in Volume 1, Case 9.
Case D:
This is a 3-month old female with fever and
coughing.
View Case D.
Interpretation of Case C
There is hyperlucency of the left chest with a
mediastinal and cardiac shift to the right. Although this
may look like a tension pneumothorax, realize that such
a large tension pneumothorax would generally be
associated with hypotension, bradycardia, and
persistent hypoxia (despite supplemental oxygen).
Since this infant appears to have good cardiovascular
function and his oxygenation improved with
supplemental oxygen, one should not immediately jump
to evacuating the left chest since he is currently stable.
After carefully reassessing the situation and
reexamining the CXR, it is evident that lung markings
are present in the left chest. This represents a
hyperexpanded lobe. The hyperexpansion is so severe
that it compresses the remaining left lung and pushes
the heart and mediastinum to the right, compressing the
right lung as well.
Impression: Left upper lobe hyperexpansion with
mediastinal shift. Congenital lobar emphysema. This
case is discussed in more detail in Volume 1, Case 9.
Case D:
This is a 3-month old female with fever and
coughing.
View Case D.
 Interpretation of Case D
This is a dark film. It is best read using a hot light.
To maximize visibility on the computer monitor, turn off
the room lights and adjust the contrast and brightness
controls on your monitor to maximize image quality.
There is a faintly visible infiltrate in the right upper
lobe. Subtle findings may be more difficult to
appreciate on dark films.
Impression: Right upper lobe infiltrate.
Case E:
This is a two month old male with a history of a VSD
(taking digoxin) arriving in the E.D. for a possible
seizure. His parents witnessed an episode of body
stiffness, jerking of all extremities, and upward rolling of
his eyes lasting one minute. An ambulance brought
him to the E.D.
His exam was significant for a harsh grade III/VI
systolic murmur. His lungs were clear. He was alert
and active, and no neurologic abnormalities could be
detected. He promptly had another generalized seizure
in the ED which lasted five minutes. An IV could not be
started during the seizure. After the seizure, he was
not drowsy. An IV was started, and he was given IV
lorazepam and phenobarbital.
View Case E.
Interpretation of Case D
This is a dark film. It is best read using a hot light.
To maximize visibility on the computer monitor, turn off
the room lights and adjust the contrast and brightness
controls on your monitor to maximize image quality.
There is a faintly visible infiltrate in the right upper
lobe. Subtle findings may be more difficult to
appreciate on dark films.
Impression: Right upper lobe infiltrate.
Case E:
This is a two month old male with a history of a VSD
(taking digoxin) arriving in the E.D. for a possible
seizure. His parents witnessed an episode of body
stiffness, jerking of all extremities, and upward rolling of
his eyes lasting one minute. An ambulance brought
him to the E.D.
His exam was significant for a harsh grade III/VI
systolic murmur. His lungs were clear. He was alert
and active, and no neurologic abnormalities could be
detected. He promptly had another generalized seizure
in the ED which lasted five minutes. An IV could not be
started during the seizure. After the seizure, he was
not drowsy. An IV was started, and he was given IV
lorazepam and phenobarbital.
View Case E.
 Interpretation of Case E
There is cardiomegaly with slightly prominent
pulmonary vascularity suggesting a left to right shunt.
An unexpected finding was the absence of a thymic
shadow that one would expect to see in a 2-month old.
A prominent thymus is usually visible in the upper
mediastinum on the AP or PA view. On the lateral
view, the space anterior and superior to the heart is
usually occupied by the thymus in this age group.
However, in this child, the thymic space is occupied by
lung tissue.
His laboratory studies were significant for
hypocalcemia. Although his clinical presentation
resembled a classic seizure, in retrospect, the
hypocalcemia suggests that these episodes were
symptomatic tetany.
Impression: Cardiomegaly and absence of the
thymic shadow. In conjunction with the VSD and
hypocalcemia, this is most consistent with DiGeorge
syndrome (thymic and hypoparathyroid aplasia or
hypoplasia). This case is discussed in more detail in
Volume 2, Case 2.
Case F:
This is a 16 year old male presenting to the
emergency department with moderately severe acute
wheezing. His oxygen saturation is 95% in room air.
He is noted to be wheezing. He is given an albuterol
aerosol and he is noted to improve, but his degree of
aeration is still somewhat poor. He complains of mild
chest pain.
View Case F.
Interpretation of Case E
There is cardiomegaly with slightly prominent
pulmonary vascularity suggesting a left to right shunt.
An unexpected finding was the absence of a thymic
shadow that one would expect to see in a 2-month old.
A prominent thymus is usually visible in the upper
mediastinum on the AP or PA view. On the lateral
view, the space anterior and superior to the heart is
usually occupied by the thymus in this age group.
However, in this child, the thymic space is occupied by
lung tissue.
His laboratory studies were significant for
hypocalcemia. Although his clinical presentation
resembled a classic seizure, in retrospect, the
hypocalcemia suggests that these episodes were
symptomatic tetany.
Impression: Cardiomegaly and absence of the
thymic shadow. In conjunction with the VSD and
hypocalcemia, this is most consistent with DiGeorge
syndrome (thymic and hypoparathyroid aplasia or
hypoplasia). This case is discussed in more detail in
Volume 2, Case 2.
Case F:
This is a 16 year old male presenting to the
emergency department with moderately severe acute
wheezing. His oxygen saturation is 95% in room air.
He is noted to be wheezing. He is given an albuterol
aerosol and he is noted to improve, but his degree of
aeration is still somewhat poor. He complains of mild
chest pain.
View Case F.
 Interpretation of Case F
Both lungs are hyperaerated. There are vertical air
densities seen in the upper mediastinum extending up
into the soft tissues of the neck. This is evidence of air
dissecting against the left border of the cardiac
silhouette. There is no evidence of pneumothorax.
Impression: Pneumomediastinum.
In a pneumomediastinum, the lateral view will often
show air dissecting along the trachea or free air may be
visible in the space anterior to the heart in the thymic
region. In this case, free air in the thymic region is
visible, but it may be difficult to see it on your computer
monitor. There are vertical oblique air densities in the
thymic space anterior and superior to the heart on the
lateral view. Darken the room and adjust the contrast
and brightness on your monitor to see it best.
Case G:
This is a 10 year old male who came to the E.D. with
a history of coughing and fever. Poor breath sounds
were noted on the left.
View Case G.
Interpretation of Case F
Both lungs are hyperaerated. There are vertical air
densities seen in the upper mediastinum extending up
into the soft tissues of the neck. This is evidence of air
dissecting against the left border of the cardiac
silhouette. There is no evidence of pneumothorax.
Impression: Pneumomediastinum.
In a pneumomediastinum, the lateral view will often
show air dissecting along the trachea or free air may be
visible in the space anterior to the heart in the thymic
region. In this case, free air in the thymic region is
visible, but it may be difficult to see it on your computer
monitor. There are vertical oblique air densities in the
thymic space anterior and superior to the heart on the
lateral view. Darken the room and adjust the contrast
and brightness on your monitor to see it best.
Case G:
This is a 10 year old male who came to the E.D. with
a history of coughing and fever. Poor breath sounds
were noted on the left.
View Case G.
 Interpretation of Case G
The left lung is consolidated. This atelectasis
results in a mediastinal shift to the left. There are air
bronchograms evident over the left lung. On the
original film, there is a suggestion of a 1.5cm cylindrical
foreign body in the left mainstem bronchus. Further
history revealed that he had "swallowed" a plastic bullet
several days ago.
Impression: Consolidation of the entire left lung with
the suggestion of a foreign body in the left mainstem
bronchus.
Case H:
This is an 11-month old female with a history of a
previous pneumonia who now presents with fever and
coughing. Mild wheezing and rales are noted on
auscultation.
View Case H.
Interpretation of Case G
The left lung is consolidated. This atelectasis
results in a mediastinal shift to the left. There are air
bronchograms evident over the left lung. On the
original film, there is a suggestion of a 1.5cm cylindrical
foreign body in the left mainstem bronchus. Further
history revealed that he had "swallowed" a plastic bullet
several days ago.
Impression: Consolidation of the entire left lung with
the suggestion of a foreign body in the left mainstem
bronchus.
Case H:
This is an 11-month old female with a history of a
previous pneumonia who now presents with fever and
coughing. Mild wheezing and rales are noted on
auscultation.
View Case H.
 Interpretation of Case H
There are small interstitial central pulmonary
infiltrates.
Impression: Small interstitial central pulmonary
infiltrates most consistent with a viral pneumonia.
Case I:
This is a 6-week old male infant. His parents
brought him to the E.D. because of coughing and
congestion. He had a 20 minute episode of frequent
coughing, but now seems to be better. He is feeding
well. There is no history of fever or cyanosis. His vital
signs are normal. Oxygen saturation is 100% in room
air. Auscultation is clear.
View Case I.
Interpretation of Case H
There are small interstitial central pulmonary
infiltrates.
Impression: Small interstitial central pulmonary
infiltrates most consistent with a viral pneumonia.
Case I:
This is a 6-week old male infant. His parents
brought him to the E.D. because of coughing and
congestion. He had a 20 minute episode of frequent
coughing, but now seems to be better. He is feeding
well. There is no history of fever or cyanosis. His vital
signs are normal. Oxygen saturation is 100% in room
air. Auscultation is clear.
View Case I.
 Interpretation of Case I
The upper mediastinum shows the usual prominent
thymus for this age. The thymic shadow is larger on
the infant's right than on his left. There is a density in
the right upper lobe, but it is obscured by the thymus.
Part of this density appears to be from the scapula, but
on close inspection, there are densities suggesting
infiltrates aside from the thymus and the scapula in the
right upper lobe.
Impression: Right upper lobe infiltrate or partial
atelectasis.
Case J:
This is an 18-month old female with a history of
prematurity and mild bronchopulmonary dysplasia. She
arrives in the emergency department with a history of
fever, coughing, and difficulty breathing. Coarse breath
sounds and mild wheezing are noted on auscultation.
View Case J.
Interpretation of Case I
The upper mediastinum shows the usual prominent
thymus for this age. The thymic shadow is larger on
the infant's right than on his left. There is a density in
the right upper lobe, but it is obscured by the thymus.
Part of this density appears to be from the scapula, but
on close inspection, there are densities suggesting
infiltrates aside from the thymus and the scapula in the
right upper lobe.
Impression: Right upper lobe infiltrate or partial
atelectasis.
Case J:
This is an 18-month old female with a history of
prematurity and mild bronchopulmonary dysplasia. She
arrives in the emergency department with a history of
fever, coughing, and difficulty breathing. Coarse breath
sounds and mild wheezing are noted on auscultation.
View Case J.
 Interpretation of Case J
There is a small area of atelectasis in the right
middle lobe. This is best seen on the lateral view as an
oblique flattened wedge shaped density over the heart.
Instead of the normal triangular shape of the right
middle lobe, it appears to be flat and compressed
indicating atelectasis.
Impression: Right middle lobe atelectasis.
Case K:
This is a 5-week old infant with a history of fever and
coughing. He arrives in the emergency department with
severe respratory distress. His initial CXR shows a
small pneumonia. He is thought to have a staph aureus
pneumonia because of his severe condition. He
requires mechanical ventilation in an intensive care unit.
During his second day of hospitalization, he suddenly
becomes severely cyanotic, bradycardic, and
hypotensive. He has good breath sounds bilaterally.
This portable CXR (AP only) is obtained.
View Case K.
Interpretation of Case J
There is a small area of atelectasis in the right
middle lobe. This is best seen on the lateral view as an
oblique flattened wedge shaped density over the heart.
Instead of the normal triangular shape of the right
middle lobe, it appears to be flat and compressed
indicating atelectasis.
Impression: Right middle lobe atelectasis.
Case K:
This is a 5-week old infant with a history of fever and
coughing. He arrives in the emergency department with
severe respratory distress. His initial CXR shows a
small pneumonia. He is thought to have a staph aureus
pneumonia because of his severe condition. He
requires mechanical ventilation in an intensive care unit.
During his second day of hospitalization, he suddenly
becomes severely cyanotic, bradycardic, and
hypotensive. He has good breath sounds bilaterally.
This portable CXR (AP only) is obtained.
View Case K.
 Interpretation of Case K
There is a lucency visible surrounding the heart;
representing air dissecting into the pericardium.
Impression: Pneumopericardium
Pneumopericardium is usually a serious emergency
since it results in sudden cardiac tamponade.
Immediate pericardiocentesis is required. This is a
highly complication prone procedure since it may
lacerate the heart and even if it temporarily relieves the
tamponade, more air will continue to accumulate in the
pericardial space resulting in recurrent tamponade.
Because of reaccumulation of air, inserting a plastic
catheter into the pericardium using an IV catheter over
needle or the Seldinger technique, may be more
effective at preventing reaccumulation of air and
tamponade. If a surgeon is immediately available, a
pericardial window procedure may be more efficacious
immediately following pericardiocentesis.
Case L:
This is an 11-year old female with a history of fever
and coughing for 5 days. VS T39.1 (oral), P122, R 20,
BP 107/76. Oxygen saturation 99% in room air.
Auscultation is significant for moist rhonchi in the left
base.
View Case L.
Interpretation of Case K
There is a lucency visible surrounding the heart;
representing air dissecting into the pericardium.
Impression: Pneumopericardium
Pneumopericardium is usually a serious emergency
since it results in sudden cardiac tamponade.
Immediate pericardiocentesis is required. This is a
highly complication prone procedure since it may
lacerate the heart and even if it temporarily relieves the
tamponade, more air will continue to accumulate in the
pericardial space resulting in recurrent tamponade.
Because of reaccumulation of air, inserting a plastic
catheter into the pericardium using an IV catheter over
needle or the Seldinger technique, may be more
effective at preventing reaccumulation of air and
tamponade. If a surgeon is immediately available, a
pericardial window procedure may be more efficacious
immediately following pericardiocentesis.
Case L:
This is an 11-year old female with a history of fever
and coughing for 5 days. VS T39.1 (oral), P122, R 20,
BP 107/76. Oxygen saturation 99% in room air.
Auscultation is significant for moist rhonchi in the left
base.
View Case L.
 Interpretation of Case L
There is a patchy infiltrate at the left lung base. This
is seen on the lateral view obliquely over the heart and
on the PA view as haziness in the left lower lung. The
prominence of the right perihilar region is probably due
to rotation. Note the asymmetry of the spinal column
and the ribs. This rotation exposes more of the right
hilum in the radiograph, making it appear more
prominent.
Impression: Patchy area of consolidation at the left
lung base.
Case M:
This is a 12-year old female complaining of a
headache and productive cough. Onset of fever last
night to 39 degrees. Rales are noted in the left base.
View Case M.
Interpretation of Case L
There is a patchy infiltrate at the left lung base. This
is seen on the lateral view obliquely over the heart and
on the PA view as haziness in the left lower lung. The
prominence of the right perihilar region is probably due
to rotation. Note the asymmetry of the spinal column
and the ribs. This rotation exposes more of the right
hilum in the radiograph, making it appear more
prominent.
Impression: Patchy area of consolidation at the left
lung base.
Case M:
This is a 12-year old female complaining of a
headache and productive cough. Onset of fever last
night to 39 degrees. Rales are noted in the left base.
View Case M.
 Interpretation of Case M
There are infiltrates in the right middle and left lower
lobes. The right middle lobe infiltrate is blurring the
right heart border. It can also be seen on the lateral
view as streakiness over the heart. The left lower lobe
infiltrate is best seen on the lateral view posteriorly on
the diaphragm. It can also be seen on the PA view as
haziness in the lower lung on the left. The infiltrate in
the right middle lobe was noted two years ago on a
previous radiograph, and the possibility of a chronic
infiltrate was raised.
Impression: Right middle and left lower lobe
infiltrates.
Case N:
This is a 9-year old male with a history of fever,
headache, nausea, and coughing.
View Case N.
Interpretation of Case M
There are infiltrates in the right middle and left lower
lobes. The right middle lobe infiltrate is blurring the
right heart border. It can also be seen on the lateral
view as streakiness over the heart. The left lower lobe
infiltrate is best seen on the lateral view posteriorly on
the diaphragm. It can also be seen on the PA view as
haziness in the lower lung on the left. The infiltrate in
the right middle lobe was noted two years ago on a
previous radiograph, and the possibility of a chronic
infiltrate was raised.
Impression: Right middle and left lower lobe
infiltrates.
Case N:
This is a 9-year old male with a history of fever,
headache, nausea, and coughing.
View Case N.
 Interpretation of Case N
There is a circular density in the right lung. This is
the superior segment of the right lower lobe. Although
this has the appearance of a mass, it is most likely an
infectious process.
Impression: Spherical consolidation in the right
lower lobe (round pneumonia).
Case O:
This is a 20-year old male who arrives in the E.D.
complaining of difficulty breathing. He also describes
some mild chest pain. He is a poor historian, but does
admit to smoking crack cocaine earlier in the day.
Auscultation reveals a "friction rub" that occurs in
synchrony with his heart rate. His pulses and perfusion
are good.
View Case O.
Interpretation of Case N
There is a circular density in the right lung. This is
the superior segment of the right lower lobe. Although
this has the appearance of a mass, it is most likely an
infectious process.
Impression: Spherical consolidation in the right
lower lobe (round pneumonia).
Case O:
This is a 20-year old male who arrives in the E.D.
complaining of difficulty breathing. He also describes
some mild chest pain. He is a poor historian, but does
admit to smoking crack cocaine earlier in the day.
Auscultation reveals a "friction rub" that occurs in
synchrony with his heart rate. His pulses and perfusion
are good.
View Case O.
 Interpretation of Case O
On the PA film, air is seen dissecting along the
superior mediastinum bilaterally. These vertical air
densities extend up into the soft tissues outside the
pleural cavity. There is also air superimposed over the
inferior aspect of the aortic arch. The lateral view
shows air densities demarcating the thymus. You may
have to darken the room and adjust the contrast and
brightness controls on your monitor to appreciate this.
The lateral view also shows vertical air densities
outlining the trachea.
Impression: Pneumomediastinum.
Pneumomediastinum is commonly associated with
substance abuse and other activities that involve a
valsalva maneuver. The "friction rub" that was
auscultated was not really a friction rub. This grating
sound called Hamman's Sign is associated with
pneumomediastinum. This case is discussed in more
detail in Volume 1, Case 7.
Case P:
This is a 17-month old female with a history of fever
and coughing. She is crying on exam making
auscultation difficult. Oxygen saturation is 98% in room
air.
View Case P.
Interpretation of Case O
On the PA film, air is seen dissecting along the
superior mediastinum bilaterally. These vertical air
densities extend up into the soft tissues outside the
pleural cavity. There is also air superimposed over the
inferior aspect of the aortic arch. The lateral view
shows air densities demarcating the thymus. You may
have to darken the room and adjust the contrast and
brightness controls on your monitor to appreciate this.
The lateral view also shows vertical air densities
outlining the trachea.
Impression: Pneumomediastinum.
Pneumomediastinum is commonly associated with
substance abuse and other activities that involve a
valsalva maneuver. The "friction rub" that was
auscultated was not really a friction rub. This grating
sound called Hamman's Sign is associated with
pneumomediastinum. This case is discussed in more
detail in Volume 1, Case 7.
Case P:
This is a 17-month old female with a history of fever
and coughing. She is crying on exam making
auscultation difficult. Oxygen saturation is 98% in room
air.
View Case P.
 Interpretation of Case P
There is a small subtle infiltrate in the left
costophrenic angle. This is best seen on the PA view
as an increased density where the ribs cross each other
in the left lower lung near the costophrenic angle.
Impression: Small infiltrate in the left costophrenic
angle.
Interpretation of Case P
There is a small subtle infiltrate in the left
costophrenic angle. This is best seen on the PA view
as an increased density where the ribs cross each other
in the left lower lung near the costophrenic angle.
Impression: Small infiltrate in the left costophrenic
angle.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Interpretation of Case A
Bilateral central pulmonary infiltrates, but most
marked in the right middle and left lower lobes. The
left lower lobe infiltrate is best seen on the lateral
view inferiorly over the spine. The lungs are
hyperaerated.
Impression: Right middle and left lower lobe
infiltrates.
Case B:
This is a 3 year old female whose parents do not
speak English well. Her chief complaint is coughing
and difficulty breathing. There is mild bilateral stridor on
exam. Her cough sounds slightly bronchospastic, but
not barking in nature.
View Case B.
Interpretation of Case A
Bilateral central pulmonary infiltrates, but most
marked in the right middle and left lower lobes. The
left lower lobe infiltrate is best seen on the lateral
view inferiorly over the spine. The lungs are
hyperaerated.
Impression: Right middle and left lower lobe
infiltrates.
Case B:
This is a 3 year old female whose parents do not
speak English well. Her chief complaint is coughing
and difficulty breathing. There is mild bilateral stridor on
exam. Her cough sounds slightly bronchospastic, but
not barking in nature.
View Case B.
 Interpretation of Case B
No infiltrates are noted. The right side is more
lucent (darker) compared to the left. This is subtle and
may be difficult to appreciate unless you step back and
view the CXR from a distance. The right
hemidiaphragm is slightly higher than the left
hemidiaphragm, however, it should be higher than this.
Both these findings suggest right sided hyperexpansion.
More clinical history through a translator indicated that
she was jumping on a bed while eating some food
(thought to be meat), when she began choking. Since
that time, she has experienced respiratory difficulty.
Further radiographs revealed bilateral air trapping.
Bronchoscopy revealed bilateral bronchial peanut
fragment foreign bodies.
Impression: Right sided hyperexpansion and air
trapping. Possible bronchial foreign body.
Case C:
This is a two week old male infant who arrived in the
E.D. with a history of noisy breathing and worsening
respiratory distress. VS T36.7, P160, R60, BP 100/70.
His color is dusky. His oxygen saturation is 86% in
room air. Oxygen is applied and his color improves.
His oxygen saturation is now 96%. He has diminished
breath sounds bilaterally. There are moderately severe
retractions.
View Case C
Interpretation of Case B
No infiltrates are noted. The right side is more
lucent (darker) compared to the left. This is subtle and
may be difficult to appreciate unless you step back and
view the CXR from a distance. The right
hemidiaphragm is slightly higher than the left
hemidiaphragm, however, it should be higher than this.
Both these findings suggest right sided hyperexpansion.
More clinical history through a translator indicated that
she was jumping on a bed while eating some food
(thought to be meat), when she began choking. Since
that time, she has experienced respiratory difficulty.
Further radiographs revealed bilateral air trapping.
Bronchoscopy revealed bilateral bronchial peanut
fragment foreign bodies.
Impression: Right sided hyperexpansion and air
trapping. Possible bronchial foreign body.
Case C:
This is a two week old male infant who arrived in the
E.D. with a history of noisy breathing and worsening
respiratory distress. VS T36.7, P160, R60, BP 100/70.
His color is dusky. His oxygen saturation is 86% in
room air. Oxygen is applied and his color improves.
His oxygen saturation is now 96%. He has diminished
breath sounds bilaterally. There are moderately severe
retractions.
View Case C
 Interpretation of Case C
There is hyperlucency of the left chest with a
mediastinal and cardiac shift to the right. Although this
may look like a tension pneumothorax, realize that such
a large tension pneumothorax would generally be
associated with hypotension, bradycardia, and
persistent hypoxia (despite supplemental oxygen).
Since this infant appears to have good cardiovascular
function and his oxygenation improved with
supplemental oxygen, one should not immediately jump
to evacuating the left chest since he is currently stable.
After carefully reassessing the situation and
reexamining the CXR, it is evident that lung markings
are present in the left chest. This represents a
hyperexpanded lobe. The hyperexpansion is so severe
that it compresses the remaining left lung and pushes
the heart and mediastinum to the right, compressing the
right lung as well.
Impression: Left upper lobe hyperexpansion with
mediastinal shift. Congenital lobar emphysema. This
case is discussed in more detail in Volume 1, Case 9.
Case D:
This is a 3-month old female with fever and
coughing.
View Case D.
Interpretation of Case C
There is hyperlucency of the left chest with a
mediastinal and cardiac shift to the right. Although this
may look like a tension pneumothorax, realize that such
a large tension pneumothorax would generally be
associated with hypotension, bradycardia, and
persistent hypoxia (despite supplemental oxygen).
Since this infant appears to have good cardiovascular
function and his oxygenation improved with
supplemental oxygen, one should not immediately jump
to evacuating the left chest since he is currently stable.
After carefully reassessing the situation and
reexamining the CXR, it is evident that lung markings
are present in the left chest. This represents a
hyperexpanded lobe. The hyperexpansion is so severe
that it compresses the remaining left lung and pushes
the heart and mediastinum to the right, compressing the
right lung as well.
Impression: Left upper lobe hyperexpansion with
mediastinal shift. Congenital lobar emphysema. This
case is discussed in more detail in Volume 1, Case 9.
Case D:
This is a 3-month old female with fever and
coughing.
View Case D.
 Interpretation of Case D
This is a dark film. It is best read using a hot light.
To maximize visibility on the computer monitor, turn off
the room lights and adjust the contrast and brightness
controls on your monitor to maximize image quality.
There is a faintly visible infiltrate in the right upper
lobe. Subtle findings may be more difficult to
appreciate on dark films.
Impression: Right upper lobe infiltrate.
Case E:
This is a two month old male with a history of a VSD
(taking digoxin) arriving in the E.D. for a possible
seizure. His parents witnessed an episode of body
stiffness, jerking of all extremities, and upward rolling of
his eyes lasting one minute. An ambulance brought
him to the E.D.
His exam was significant for a harsh grade III/VI
systolic murmur. His lungs were clear. He was alert
and active, and no neurologic abnormalities could be
detected. He promptly had another generalized seizure
in the ED which lasted five minutes. An IV could not be
started during the seizure. After the seizure, he was
not drowsy. An IV was started, and he was given IV
lorazepam and phenobarbital.
View Case E.
Interpretation of Case D
This is a dark film. It is best read using a hot light.
To maximize visibility on the computer monitor, turn off
the room lights and adjust the contrast and brightness
controls on your monitor to maximize image quality.
There is a faintly visible infiltrate in the right upper
lobe. Subtle findings may be more difficult to
appreciate on dark films.
Impression: Right upper lobe infiltrate.
Case E:
This is a two month old male with a history of a VSD
(taking digoxin) arriving in the E.D. for a possible
seizure. His parents witnessed an episode of body
stiffness, jerking of all extremities, and upward rolling of
his eyes lasting one minute. An ambulance brought
him to the E.D.
His exam was significant for a harsh grade III/VI
systolic murmur. His lungs were clear. He was alert
and active, and no neurologic abnormalities could be
detected. He promptly had another generalized seizure
in the ED which lasted five minutes. An IV could not be
started during the seizure. After the seizure, he was
not drowsy. An IV was started, and he was given IV
lorazepam and phenobarbital.
View Case E.
 Interpretation of Case E
There is cardiomegaly with slightly prominent
pulmonary vascularity suggesting a left to right shunt.
An unexpected finding was the absence of a thymic
shadow that one would expect to see in a 2-month old.
A prominent thymus is usually visible in the upper
mediastinum on the AP or PA view. On the lateral
view, the space anterior and superior to the heart is
usually occupied by the thymus in this age group.
However, in this child, the thymic space is occupied by
lung tissue.
His laboratory studies were significant for
hypocalcemia. Although his clinical presentation
resembled a classic seizure, in retrospect, the
hypocalcemia suggests that these episodes were
symptomatic tetany.
Impression: Cardiomegaly and absence of the
thymic shadow. In conjunction with the VSD and
hypocalcemia, this is most consistent with DiGeorge
syndrome (thymic and hypoparathyroid aplasia or
hypoplasia). This case is discussed in more detail in
Volume 2, Case 2.
Case F:
This is a 16 year old male presenting to the
emergency department with moderately severe acute
wheezing. His oxygen saturation is 95% in room air.
He is noted to be wheezing. He is given an albuterol
aerosol and he is noted to improve, but his degree of
aeration is still somewhat poor. He complains of mild
chest pain.
View Case F.
Interpretation of Case E
There is cardiomegaly with slightly prominent
pulmonary vascularity suggesting a left to right shunt.
An unexpected finding was the absence of a thymic
shadow that one would expect to see in a 2-month old.
A prominent thymus is usually visible in the upper
mediastinum on the AP or PA view. On the lateral
view, the space anterior and superior to the heart is
usually occupied by the thymus in this age group.
However, in this child, the thymic space is occupied by
lung tissue.
His laboratory studies were significant for
hypocalcemia. Although his clinical presentation
resembled a classic seizure, in retrospect, the
hypocalcemia suggests that these episodes were
symptomatic tetany.
Impression: Cardiomegaly and absence of the
thymic shadow. In conjunction with the VSD and
hypocalcemia, this is most consistent with DiGeorge
syndrome (thymic and hypoparathyroid aplasia or
hypoplasia). This case is discussed in more detail in
Volume 2, Case 2.
Case F:
This is a 16 year old male presenting to the
emergency department with moderately severe acute
wheezing. His oxygen saturation is 95% in room air.
He is noted to be wheezing. He is given an albuterol
aerosol and he is noted to improve, but his degree of
aeration is still somewhat poor. He complains of mild
chest pain.
View Case F.
 Interpretation of Case F
Both lungs are hyperaerated. There are vertical air
densities seen in the upper mediastinum extending up
into the soft tissues of the neck. This is evidence of air
dissecting against the left border of the cardiac
silhouette. There is no evidence of pneumothorax.
Impression: Pneumomediastinum.
In a pneumomediastinum, the lateral view will often
show air dissecting along the trachea or free air may be
visible in the space anterior to the heart in the thymic
region. In this case, free air in the thymic region is
visible, but it may be difficult to see it on your computer
monitor. There are vertical oblique air densities in the
thymic space anterior and superior to the heart on the
lateral view. Darken the room and adjust the contrast
and brightness on your monitor to see it best.
Case G:
This is a 10 year old male who came to the E.D. with
a history of coughing and fever. Poor breath sounds
were noted on the left.
View Case G.
Interpretation of Case F
Both lungs are hyperaerated. There are vertical air
densities seen in the upper mediastinum extending up
into the soft tissues of the neck. This is evidence of air
dissecting against the left border of the cardiac
silhouette. There is no evidence of pneumothorax.
Impression: Pneumomediastinum.
In a pneumomediastinum, the lateral view will often
show air dissecting along the trachea or free air may be
visible in the space anterior to the heart in the thymic
region. In this case, free air in the thymic region is
visible, but it may be difficult to see it on your computer
monitor. There are vertical oblique air densities in the
thymic space anterior and superior to the heart on the
lateral view. Darken the room and adjust the contrast
and brightness on your monitor to see it best.
Case G:
This is a 10 year old male who came to the E.D. with
a history of coughing and fever. Poor breath sounds
were noted on the left.
View Case G.
 Interpretation of Case G
The left lung is consolidated. This atelectasis
results in a mediastinal shift to the left. There are air
bronchograms evident over the left lung. On the
original film, there is a suggestion of a 1.5cm cylindrical
foreign body in the left mainstem bronchus. Further
history revealed that he had "swallowed" a plastic bullet
several days ago.
Impression: Consolidation of the entire left lung with
the suggestion of a foreign body in the left mainstem
bronchus.
Case H:
This is an 11-month old female with a history of a
previous pneumonia who now presents with fever and
coughing. Mild wheezing and rales are noted on
auscultation.
View Case H.
Interpretation of Case G
The left lung is consolidated. This atelectasis
results in a mediastinal shift to the left. There are air
bronchograms evident over the left lung. On the
original film, there is a suggestion of a 1.5cm cylindrical
foreign body in the left mainstem bronchus. Further
history revealed that he had "swallowed" a plastic bullet
several days ago.
Impression: Consolidation of the entire left lung with
the suggestion of a foreign body in the left mainstem
bronchus.
Case H:
This is an 11-month old female with a history of a
previous pneumonia who now presents with fever and
coughing. Mild wheezing and rales are noted on
auscultation.
View Case H.
 Interpretation of Case H
There are small interstitial central pulmonary
infiltrates.
Impression: Small interstitial central pulmonary
infiltrates most consistent with a viral pneumonia.
Case I:
This is a 6-week old male infant. His parents
brought him to the E.D. because of coughing and
congestion. He had a 20 minute episode of frequent
coughing, but now seems to be better. He is feeding
well. There is no history of fever or cyanosis. His vital
signs are normal. Oxygen saturation is 100% in room
air. Auscultation is clear.
View Case I.
Interpretation of Case H
There are small interstitial central pulmonary
infiltrates.
Impression: Small interstitial central pulmonary
infiltrates most consistent with a viral pneumonia.
Case I:
This is a 6-week old male infant. His parents
brought him to the E.D. because of coughing and
congestion. He had a 20 minute episode of frequent
coughing, but now seems to be better. He is feeding
well. There is no history of fever or cyanosis. His vital
signs are normal. Oxygen saturation is 100% in room
air. Auscultation is clear.
View Case I.
 Interpretation of Case I
The upper mediastinum shows the usual prominent
thymus for this age. The thymic shadow is larger on
the infant's right than on his left. There is a density in
the right upper lobe, but it is obscured by the thymus.
Part of this density appears to be from the scapula, but
on close inspection, there are densities suggesting
infiltrates aside from the thymus and the scapula in the
right upper lobe.
Impression: Right upper lobe infiltrate or partial
atelectasis.
Case J:
This is an 18-month old female with a history of
prematurity and mild bronchopulmonary dysplasia. She
arrives in the emergency department with a history of
fever, coughing, and difficulty breathing. Coarse breath
sounds and mild wheezing are noted on auscultation.
View Case J.
Interpretation of Case I
The upper mediastinum shows the usual prominent
thymus for this age. The thymic shadow is larger on
the infant's right than on his left. There is a density in
the right upper lobe, but it is obscured by the thymus.
Part of this density appears to be from the scapula, but
on close inspection, there are densities suggesting
infiltrates aside from the thymus and the scapula in the
right upper lobe.
Impression: Right upper lobe infiltrate or partial
atelectasis.
Case J:
This is an 18-month old female with a history of
prematurity and mild bronchopulmonary dysplasia. She
arrives in the emergency department with a history of
fever, coughing, and difficulty breathing. Coarse breath
sounds and mild wheezing are noted on auscultation.
View Case J.
 Interpretation of Case J
There is a small area of atelectasis in the right
middle lobe. This is best seen on the lateral view as an
oblique flattened wedge shaped density over the heart.
Instead of the normal triangular shape of the right
middle lobe, it appears to be flat and compressed
indicating atelectasis.
Impression: Right middle lobe atelectasis.
Case K:
This is a 5-week old infant with a history of fever and
coughing. He arrives in the emergency department with
severe respratory distress. His initial CXR shows a
small pneumonia. He is thought to have a staph aureus
pneumonia because of his severe condition. He
requires mechanical ventilation in an intensive care unit.
During his second day of hospitalization, he suddenly
becomes severely cyanotic, bradycardic, and
hypotensive. He has good breath sounds bilaterally.
This portable CXR (AP only) is obtained.
View Case K.
Interpretation of Case J
There is a small area of atelectasis in the right
middle lobe. This is best seen on the lateral view as an
oblique flattened wedge shaped density over the heart.
Instead of the normal triangular shape of the right
middle lobe, it appears to be flat and compressed
indicating atelectasis.
Impression: Right middle lobe atelectasis.
Case K:
This is a 5-week old infant with a history of fever and
coughing. He arrives in the emergency department with
severe respratory distress. His initial CXR shows a
small pneumonia. He is thought to have a staph aureus
pneumonia because of his severe condition. He
requires mechanical ventilation in an intensive care unit.
During his second day of hospitalization, he suddenly
becomes severely cyanotic, bradycardic, and
hypotensive. He has good breath sounds bilaterally.
This portable CXR (AP only) is obtained.
View Case K.
 Interpretation of Case K
There is a lucency visible surrounding the heart;
representing air dissecting into the pericardium.
Impression: Pneumopericardium
Pneumopericardium is usually a serious emergency
since it results in sudden cardiac tamponade.
Immediate pericardiocentesis is required. This is a
highly complication prone procedure since it may
lacerate the heart and even if it temporarily relieves the
tamponade, more air will continue to accumulate in the
pericardial space resulting in recurrent tamponade.
Because of reaccumulation of air, inserting a plastic
catheter into the pericardium using an IV catheter over
needle or the Seldinger technique, may be more
effective at preventing reaccumulation of air and
tamponade. If a surgeon is immediately available, a
pericardial window procedure may be more efficacious
immediately following pericardiocentesis.
Case L:
This is an 11-year old female with a history of fever
and coughing for 5 days. VS T39.1 (oral), P122, R 20,
BP 107/76. Oxygen saturation 99% in room air.
Auscultation is significant for moist rhonchi in the left
base.
View Case L.
Interpretation of Case K
There is a lucency visible surrounding the heart;
representing air dissecting into the pericardium.
Impression: Pneumopericardium
Pneumopericardium is usually a serious emergency
since it results in sudden cardiac tamponade.
Immediate pericardiocentesis is required. This is a
highly complication prone procedure since it may
lacerate the heart and even if it temporarily relieves the
tamponade, more air will continue to accumulate in the
pericardial space resulting in recurrent tamponade.
Because of reaccumulation of air, inserting a plastic
catheter into the pericardium using an IV catheter over
needle or the Seldinger technique, may be more
effective at preventing reaccumulation of air and
tamponade. If a surgeon is immediately available, a
pericardial window procedure may be more efficacious
immediately following pericardiocentesis.
Case L:
This is an 11-year old female with a history of fever
and coughing for 5 days. VS T39.1 (oral), P122, R 20,
BP 107/76. Oxygen saturation 99% in room air.
Auscultation is significant for moist rhonchi in the left
base.
View Case L.
 Interpretation of Case L
There is a patchy infiltrate at the left lung base. This
is seen on the lateral view obliquely over the heart and
on the PA view as haziness in the left lower lung. The
prominence of the right perihilar region is probably due
to rotation. Note the asymmetry of the spinal column
and the ribs. This rotation exposes more of the right
hilum in the radiograph, making it appear more
prominent.
Impression: Patchy area of consolidation at the left
lung base.
Case M:
This is a 12-year old female complaining of a
headache and productive cough. Onset of fever last
night to 39 degrees. Rales are noted in the left base.
View Case M.
Interpretation of Case L
There is a patchy infiltrate at the left lung base. This
is seen on the lateral view obliquely over the heart and
on the PA view as haziness in the left lower lung. The
prominence of the right perihilar region is probably due
to rotation. Note the asymmetry of the spinal column
and the ribs. This rotation exposes more of the right
hilum in the radiograph, making it appear more
prominent.
Impression: Patchy area of consolidation at the left
lung base.
Case M:
This is a 12-year old female complaining of a
headache and productive cough. Onset of fever last
night to 39 degrees. Rales are noted in the left base.
View Case M.
 Interpretation of Case M
There are infiltrates in the right middle and left lower
lobes. The right middle lobe infiltrate is blurring the
right heart border. It can also be seen on the lateral
view as streakiness over the heart. The left lower lobe
infiltrate is best seen on the lateral view posteriorly on
the diaphragm. It can also be seen on the PA view as
haziness in the lower lung on the left. The infiltrate in
the right middle lobe was noted two years ago on a
previous radiograph, and the possibility of a chronic
infiltrate was raised.
Impression: Right middle and left lower lobe
infiltrates.
Case N:
This is a 9-year old male with a history of fever,
headache, nausea, and coughing.
View Case N.
Interpretation of Case M
There are infiltrates in the right middle and left lower
lobes. The right middle lobe infiltrate is blurring the
right heart border. It can also be seen on the lateral
view as streakiness over the heart. The left lower lobe
infiltrate is best seen on the lateral view posteriorly on
the diaphragm. It can also be seen on the PA view as
haziness in the lower lung on the left. The infiltrate in
the right middle lobe was noted two years ago on a
previous radiograph, and the possibility of a chronic
infiltrate was raised.
Impression: Right middle and left lower lobe
infiltrates.
Case N:
This is a 9-year old male with a history of fever,
headache, nausea, and coughing.
View Case N.
 Interpretation of Case N
There is a circular density in the right lung. This is
the superior segment of the right lower lobe. Although
this has the appearance of a mass, it is most likely an
infectious process.
Impression: Spherical consolidation in the right
lower lobe (round pneumonia).
Case O:
This is a 20-year old male who arrives in the E.D.
complaining of difficulty breathing. He also describes
some mild chest pain. He is a poor historian, but does
admit to smoking crack cocaine earlier in the day.
Auscultation reveals a "friction rub" that occurs in
synchrony with his heart rate. His pulses and perfusion
are good.
View Case O.
Interpretation of Case N
There is a circular density in the right lung. This is
the superior segment of the right lower lobe. Although
this has the appearance of a mass, it is most likely an
infectious process.
Impression: Spherical consolidation in the right
lower lobe (round pneumonia).
Case O:
This is a 20-year old male who arrives in the E.D.
complaining of difficulty breathing. He also describes
some mild chest pain. He is a poor historian, but does
admit to smoking crack cocaine earlier in the day.
Auscultation reveals a "friction rub" that occurs in
synchrony with his heart rate. His pulses and perfusion
are good.
View Case O.
 Interpretation of Case O
On the PA film, air is seen dissecting along the
superior mediastinum bilaterally. These vertical air
densities extend up into the soft tissues outside the
pleural cavity. There is also air superimposed over the
inferior aspect of the aortic arch. The lateral view
shows air densities demarcating the thymus. You may
have to darken the room and adjust the contrast and
brightness controls on your monitor to appreciate this.
The lateral view also shows vertical air densities
outlining the trachea.
Impression: Pneumomediastinum.
Pneumomediastinum is commonly associated with
substance abuse and other activities that involve a
valsalva maneuver. The "friction rub" that was
auscultated was not really a friction rub. This grating
sound called Hamman's Sign is associated with
pneumomediastinum. This case is discussed in more
detail in Volume 1, Case 7.
Case P:
This is a 17-month old female with a history of fever
and coughing. She is crying on exam making
auscultation difficult. Oxygen saturation is 98% in room
air.
View Case P.
Interpretation of Case O
On the PA film, air is seen dissecting along the
superior mediastinum bilaterally. These vertical air
densities extend up into the soft tissues outside the
pleural cavity. There is also air superimposed over the
inferior aspect of the aortic arch. The lateral view
shows air densities demarcating the thymus. You may
have to darken the room and adjust the contrast and
brightness controls on your monitor to appreciate this.
The lateral view also shows vertical air densities
outlining the trachea.
Impression: Pneumomediastinum.
Pneumomediastinum is commonly associated with
substance abuse and other activities that involve a
valsalva maneuver. The "friction rub" that was
auscultated was not really a friction rub. This grating
sound called Hamman's Sign is associated with
pneumomediastinum. This case is discussed in more
detail in Volume 1, Case 7.
Case P:
This is a 17-month old female with a history of fever
and coughing. She is crying on exam making
auscultation difficult. Oxygen saturation is 98% in room
air.
View Case P.
 Interpretation of Case P
There is a small subtle infiltrate in the left
costophrenic angle. This is best seen on the PA view
as an increased density where the ribs cross each other
in the left lower lung near the costophrenic angle.
Impression: Small infiltrate in the left costophrenic
angle.
Interpretation of Case P
There is a small subtle infiltrate in the left
costophrenic angle. This is best seen on the PA view
as an increased density where the ribs cross each other
in the left lower lung near the costophrenic angle.
Impression: Small infiltrate in the left costophrenic
angle.