Acute Chest Pain in a Tall Slender Teenager
Radiology Cases in Pediatric Emergency Medicine
Volume 3, Case 13
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 15-year old male presents to the E.D. with a one
hour history of pain in his chest and back occurring
after lifting his mother. He describes the pain as
knife-like and non radiating. His pain worsens with
deep inspiration. His pain is currently less severe than
at onset. He has a past history of chest pain episodes,
usually at night while sleeping in bed.
Exam VS T37 (tympanic), P76, R24, BP 131/65.
Oxygen saturation 100% in room air. He is alert and
active in no distress. He is tall and thin. Heart regular,
no murmurs. Lungs clear, but diminished breath
sounds bilaterally. Abdomen benign. Peripheral pulses
are full. Color and perfusion are good. Hands
significant for long thin fingers (arachnodactyly).
A chest radiograph is ordered.
View CXR.
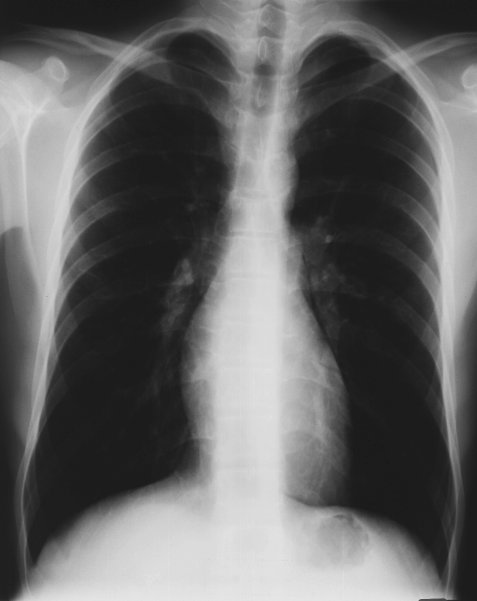 This CXR shows a long thorax with hyperexpanded
lungs. The aortic shadow is not obviously widened.
The cardiac silhouette is not enlarged. There is no
obvious pneumothorax, pneumomediastinum, or
subcutaneous emphysema.
Aortic dissection is suspected because of his
Marfanoid appearance. A CT scan of the chest and
aorta is ordered.
View CT scan.
This CXR shows a long thorax with hyperexpanded
lungs. The aortic shadow is not obviously widened.
The cardiac silhouette is not enlarged. There is no
obvious pneumothorax, pneumomediastinum, or
subcutaneous emphysema.
Aortic dissection is suspected because of his
Marfanoid appearance. A CT scan of the chest and
aorta is ordered.
View CT scan.
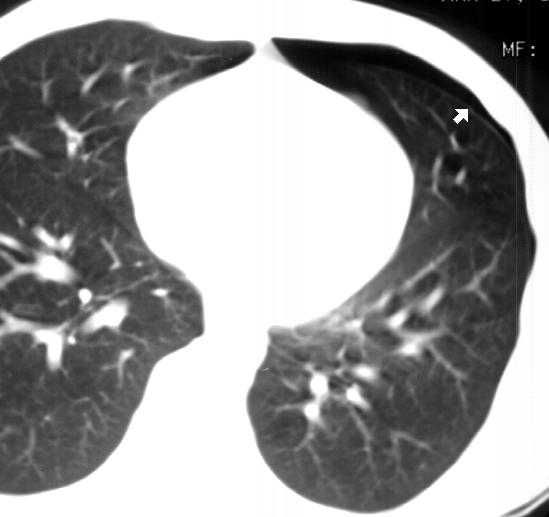 The CT scan demonstrates a small left-sided
pneumothorax. The arrows point to the visceral pleura
of the lung. An air space is evident within the pleural
space. The aorta is normal.
Upon closer inspection of subsequent CXR's, the
pneumothorax is visible as a thin rim of air over the
apex of the left lung. It is more obvious on erect and
expiratory views. Pneumothoraces may be difficult to
see on a supine or a partially supine film. The patient
should be upright or in the lateral decubitus position to
see it best.
View close-up of left apex and expiratory view.
The CT scan demonstrates a small left-sided
pneumothorax. The arrows point to the visceral pleura
of the lung. An air space is evident within the pleural
space. The aorta is normal.
Upon closer inspection of subsequent CXR's, the
pneumothorax is visible as a thin rim of air over the
apex of the left lung. It is more obvious on erect and
expiratory views. Pneumothoraces may be difficult to
see on a supine or a partially supine film. The patient
should be upright or in the lateral decubitus position to
see it best.
View close-up of left apex and expiratory view.
 After reviewing the previous case of aortic
dissection, chest pain in a tall slender patient
suggesting Marfan's Syndrome, is highly suggestive of
another aortic dissection. Marfan's Syndrome is a
connective tissue disorder prone to aortic dissection.
Patients with Marfan's Syndrome classically have a
body stature similar to that of Abraham Lincoln.
Although such tall slender individuals with chest pain
raise the possibility of aortic dissection, such individuals
are also at a higher risk of a spontaneous
pneumothorax. Other activities associated with an
increased risk of air leaks include coughing, valsalva
maneuvers (eg., musical instrument playing and
carrying one's mother), substance abuse, positive
pressure devices, etc. Patients with chronic lung
disease such as bronchopulmonary dysplasia, cystic
fibrosis, bronchiectasis, metastatic disease, etc., are at
greater risk for a spontaneous pneumothorax.
Patients with a spontaneous pneumothorax may
present with chest pain or symptoms of respiratory
difficulty. The chest pain may be similar to that of chest
wall pain in that the pain is usually worse when taking in
a deep breath. Crepitance may be palpable if air is
dissecting into the soft tissues of the neck or the chest
wall. Diminished breath sounds may be noticeable if
the pneumothorax is large enough. Small
pneumothoraces may not be detectable by auscultation.
An immediate chest tube is indicated only if the
patient is in severe distress. Otherwise, it may be best
to obtain a chest radiograph to establish a diagnosis
before performing an invasive procedure. This
pneumothorax was difficult to see on this recumbent
CXR view. If a pneumothorax is still suspected, an
expiratory erect view would accentuate the radiographic
findings, making it easier to identify a small
pneumothorax. As demonstrated in this case, CT scan
is very sensitive at identifying a pneumothorax, but it is
usually not necessary since pneumothoraces can
usually be identified on plain radiographs.
If the pneumothorax is small and the patient is doing
well, it is usually not necessary to evacuate it with a
thoracentesis or a tube thoracostomy. If no
deterioration is noted during an observation period in
the emergency department (that meets with the comfort
level of the physician and family), it may not be
necessary to hospitalize the patient (especially with
teenagers) with a small pneumothorax, if follow-up is
reliable and the family lives near a medical facility.
Elective consultation with a surgeon may be beneficial if
a tube thoracostomy is anticipated.
References
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, MD, Williams and
Wilkins, 1993, pp. 1348-1349.
After reviewing the previous case of aortic
dissection, chest pain in a tall slender patient
suggesting Marfan's Syndrome, is highly suggestive of
another aortic dissection. Marfan's Syndrome is a
connective tissue disorder prone to aortic dissection.
Patients with Marfan's Syndrome classically have a
body stature similar to that of Abraham Lincoln.
Although such tall slender individuals with chest pain
raise the possibility of aortic dissection, such individuals
are also at a higher risk of a spontaneous
pneumothorax. Other activities associated with an
increased risk of air leaks include coughing, valsalva
maneuvers (eg., musical instrument playing and
carrying one's mother), substance abuse, positive
pressure devices, etc. Patients with chronic lung
disease such as bronchopulmonary dysplasia, cystic
fibrosis, bronchiectasis, metastatic disease, etc., are at
greater risk for a spontaneous pneumothorax.
Patients with a spontaneous pneumothorax may
present with chest pain or symptoms of respiratory
difficulty. The chest pain may be similar to that of chest
wall pain in that the pain is usually worse when taking in
a deep breath. Crepitance may be palpable if air is
dissecting into the soft tissues of the neck or the chest
wall. Diminished breath sounds may be noticeable if
the pneumothorax is large enough. Small
pneumothoraces may not be detectable by auscultation.
An immediate chest tube is indicated only if the
patient is in severe distress. Otherwise, it may be best
to obtain a chest radiograph to establish a diagnosis
before performing an invasive procedure. This
pneumothorax was difficult to see on this recumbent
CXR view. If a pneumothorax is still suspected, an
expiratory erect view would accentuate the radiographic
findings, making it easier to identify a small
pneumothorax. As demonstrated in this case, CT scan
is very sensitive at identifying a pneumothorax, but it is
usually not necessary since pneumothoraces can
usually be identified on plain radiographs.
If the pneumothorax is small and the patient is doing
well, it is usually not necessary to evacuate it with a
thoracentesis or a tube thoracostomy. If no
deterioration is noted during an observation period in
the emergency department (that meets with the comfort
level of the physician and family), it may not be
necessary to hospitalize the patient (especially with
teenagers) with a small pneumothorax, if follow-up is
reliable and the family lives near a medical facility.
Elective consultation with a surgeon may be beneficial if
a tube thoracostomy is anticipated.
References
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, MD, Williams and
Wilkins, 1993, pp. 1348-1349.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
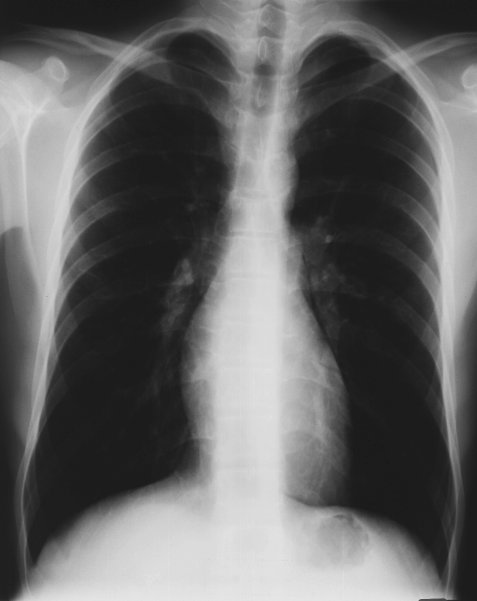 This CXR shows a long thorax with hyperexpanded
lungs. The aortic shadow is not obviously widened.
The cardiac silhouette is not enlarged. There is no
obvious pneumothorax, pneumomediastinum, or
subcutaneous emphysema.
Aortic dissection is suspected because of his
Marfanoid appearance. A CT scan of the chest and
aorta is ordered.
View CT scan.
This CXR shows a long thorax with hyperexpanded
lungs. The aortic shadow is not obviously widened.
The cardiac silhouette is not enlarged. There is no
obvious pneumothorax, pneumomediastinum, or
subcutaneous emphysema.
Aortic dissection is suspected because of his
Marfanoid appearance. A CT scan of the chest and
aorta is ordered.
View CT scan.
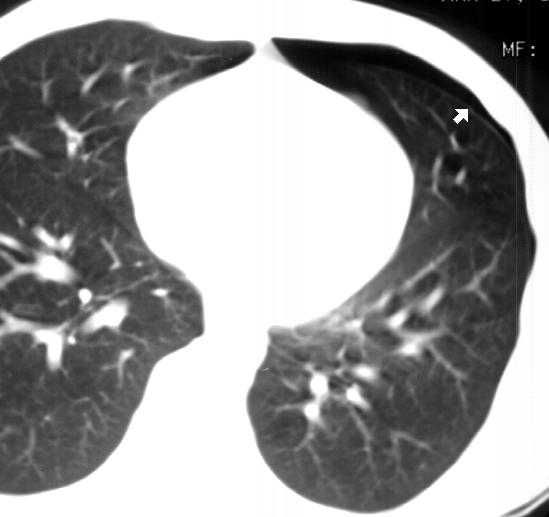 The CT scan demonstrates a small left-sided
pneumothorax. The arrows point to the visceral pleura
of the lung. An air space is evident within the pleural
space. The aorta is normal.
Upon closer inspection of subsequent CXR's, the
pneumothorax is visible as a thin rim of air over the
apex of the left lung. It is more obvious on erect and
expiratory views. Pneumothoraces may be difficult to
see on a supine or a partially supine film. The patient
should be upright or in the lateral decubitus position to
see it best.
View close-up of left apex and expiratory view.
The CT scan demonstrates a small left-sided
pneumothorax. The arrows point to the visceral pleura
of the lung. An air space is evident within the pleural
space. The aorta is normal.
Upon closer inspection of subsequent CXR's, the
pneumothorax is visible as a thin rim of air over the
apex of the left lung. It is more obvious on erect and
expiratory views. Pneumothoraces may be difficult to
see on a supine or a partially supine film. The patient
should be upright or in the lateral decubitus position to
see it best.
View close-up of left apex and expiratory view.
 After reviewing the previous case of aortic
dissection, chest pain in a tall slender patient
suggesting Marfan's Syndrome, is highly suggestive of
another aortic dissection. Marfan's Syndrome is a
connective tissue disorder prone to aortic dissection.
Patients with Marfan's Syndrome classically have a
body stature similar to that of Abraham Lincoln.
Although such tall slender individuals with chest pain
raise the possibility of aortic dissection, such individuals
are also at a higher risk of a spontaneous
pneumothorax. Other activities associated with an
increased risk of air leaks include coughing, valsalva
maneuvers (eg., musical instrument playing and
carrying one's mother), substance abuse, positive
pressure devices, etc. Patients with chronic lung
disease such as bronchopulmonary dysplasia, cystic
fibrosis, bronchiectasis, metastatic disease, etc., are at
greater risk for a spontaneous pneumothorax.
Patients with a spontaneous pneumothorax may
present with chest pain or symptoms of respiratory
difficulty. The chest pain may be similar to that of chest
wall pain in that the pain is usually worse when taking in
a deep breath. Crepitance may be palpable if air is
dissecting into the soft tissues of the neck or the chest
wall. Diminished breath sounds may be noticeable if
the pneumothorax is large enough. Small
pneumothoraces may not be detectable by auscultation.
An immediate chest tube is indicated only if the
patient is in severe distress. Otherwise, it may be best
to obtain a chest radiograph to establish a diagnosis
before performing an invasive procedure. This
pneumothorax was difficult to see on this recumbent
CXR view. If a pneumothorax is still suspected, an
expiratory erect view would accentuate the radiographic
findings, making it easier to identify a small
pneumothorax. As demonstrated in this case, CT scan
is very sensitive at identifying a pneumothorax, but it is
usually not necessary since pneumothoraces can
usually be identified on plain radiographs.
If the pneumothorax is small and the patient is doing
well, it is usually not necessary to evacuate it with a
thoracentesis or a tube thoracostomy. If no
deterioration is noted during an observation period in
the emergency department (that meets with the comfort
level of the physician and family), it may not be
necessary to hospitalize the patient (especially with
teenagers) with a small pneumothorax, if follow-up is
reliable and the family lives near a medical facility.
Elective consultation with a surgeon may be beneficial if
a tube thoracostomy is anticipated.
References
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, MD, Williams and
Wilkins, 1993, pp. 1348-1349.
After reviewing the previous case of aortic
dissection, chest pain in a tall slender patient
suggesting Marfan's Syndrome, is highly suggestive of
another aortic dissection. Marfan's Syndrome is a
connective tissue disorder prone to aortic dissection.
Patients with Marfan's Syndrome classically have a
body stature similar to that of Abraham Lincoln.
Although such tall slender individuals with chest pain
raise the possibility of aortic dissection, such individuals
are also at a higher risk of a spontaneous
pneumothorax. Other activities associated with an
increased risk of air leaks include coughing, valsalva
maneuvers (eg., musical instrument playing and
carrying one's mother), substance abuse, positive
pressure devices, etc. Patients with chronic lung
disease such as bronchopulmonary dysplasia, cystic
fibrosis, bronchiectasis, metastatic disease, etc., are at
greater risk for a spontaneous pneumothorax.
Patients with a spontaneous pneumothorax may
present with chest pain or symptoms of respiratory
difficulty. The chest pain may be similar to that of chest
wall pain in that the pain is usually worse when taking in
a deep breath. Crepitance may be palpable if air is
dissecting into the soft tissues of the neck or the chest
wall. Diminished breath sounds may be noticeable if
the pneumothorax is large enough. Small
pneumothoraces may not be detectable by auscultation.
An immediate chest tube is indicated only if the
patient is in severe distress. Otherwise, it may be best
to obtain a chest radiograph to establish a diagnosis
before performing an invasive procedure. This
pneumothorax was difficult to see on this recumbent
CXR view. If a pneumothorax is still suspected, an
expiratory erect view would accentuate the radiographic
findings, making it easier to identify a small
pneumothorax. As demonstrated in this case, CT scan
is very sensitive at identifying a pneumothorax, but it is
usually not necessary since pneumothoraces can
usually be identified on plain radiographs.
If the pneumothorax is small and the patient is doing
well, it is usually not necessary to evacuate it with a
thoracentesis or a tube thoracostomy. If no
deterioration is noted during an observation period in
the emergency department (that meets with the comfort
level of the physician and family), it may not be
necessary to hospitalize the patient (especially with
teenagers) with a small pneumothorax, if follow-up is
reliable and the family lives near a medical facility.
Elective consultation with a surgeon may be beneficial if
a tube thoracostomy is anticipated.
References
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, MD, Williams and
Wilkins, 1993, pp. 1348-1349.