Wheezing and Cyanosis in a 16-Month Old
Radiology Cases in Pediatric Emergency Medicine
Volume 2, Case 3
Collin S. Goto, M.D.
Children's Medical Center of Dallas
University of Texas Southwestern School of Medicine
The patient is a 16 month old male who presents to
the Emergency Department with a one day history of
coughing, congestion, and runny nose. His only
medications were acetaminophen and a cough syrup.
He was seen by his primary physician and instructed to
go to the E.D. His mother stated that he had a heart
murmur, for which he had been seen by a cardiologist
and told that he had a hole in his heart that would close
on its own. He had no other medical problems, no
previous surgeries, and had been doing well until the
current illness.
Exam: VS T37.1R, P170, R48, BP 112/74, oxygen
saturation 78% on room air. The patient appeared pale
and irritable, with moderate respiratory distress.
Peripheral and central cyanosis were present. Diffuse
wheezes were heard bilaterally. The precordium was
hyperdynamic, and a grade III/VI holosystolic murmur
was present, loudest along the left sternal border. The
abdomen was soft, with no organomegaly. Peripheral
pulses were brisk.
The patient was treated with 100% oxygen,
subcutaneous terbutaline, and albuterol aerosols. A
peripheral IV was placed. The patient's oxygen
saturation decreased to the 50's with crying, but
returned to the 70's when he was calmed down. He
was placed in the knee-chest position and a dose of
morphine was given IV. A 20cc/kg bolus of normal
saline was given IV. He continued to have inspiratory
and expiratory wheezes. Albuterol and ipratropium
bromide aerosols were given. A CXR and an EKG
were done.
View EKG.
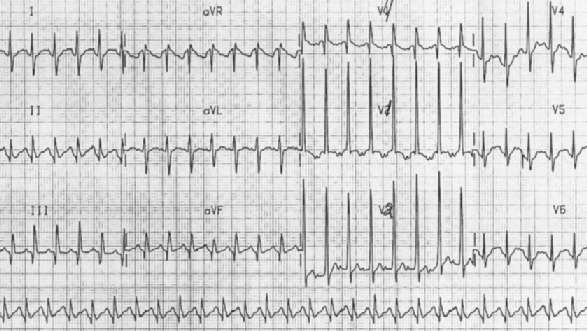
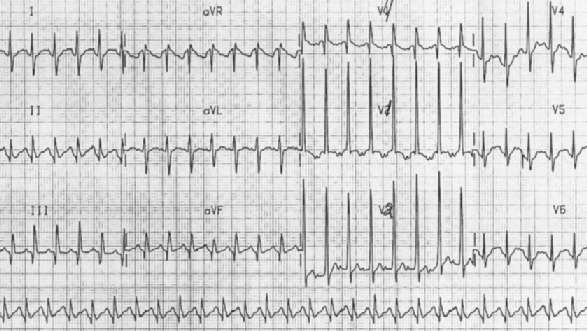 Determine the axis of QRS in the frontal plane
(using the limb leads). Note that several leads are
isoelectric (I, AVF, and AVL). Since I and AVF are
perpendicular to each other, this represents misplaced
leads or the axis is perpendicular to both leads (ie., an
anterior or posterior axis). The cardiologist reviewing
this EKG noted the axis to be "indeterminate",
indicating that the axis of QRS is largely perpendicular
to the frontal plane. The cardiologist has re-labeled
leads V1-V3. Regardless of this change, it appears that
the axis of QRS is anterior since V1 and V2 are greatly
positive (large R waves). The large R waves in lead
V1, V2, and V3 meet voltage criteria for right ventricular
hypertrophy. Although RVH usually has a right axis in
the frontal plane (greater than 90 degrees), the right
ventricle is anterior; thus, it may have an anterior
axis as well. Although RVH is normal for a newborn,
RVH is not normal for a 16-month old child.
View CXR image.
Determine the axis of QRS in the frontal plane
(using the limb leads). Note that several leads are
isoelectric (I, AVF, and AVL). Since I and AVF are
perpendicular to each other, this represents misplaced
leads or the axis is perpendicular to both leads (ie., an
anterior or posterior axis). The cardiologist reviewing
this EKG noted the axis to be "indeterminate",
indicating that the axis of QRS is largely perpendicular
to the frontal plane. The cardiologist has re-labeled
leads V1-V3. Regardless of this change, it appears that
the axis of QRS is anterior since V1 and V2 are greatly
positive (large R waves). The large R waves in lead
V1, V2, and V3 meet voltage criteria for right ventricular
hypertrophy. Although RVH usually has a right axis in
the frontal plane (greater than 90 degrees), the right
ventricle is anterior; thus, it may have an anterior
axis as well. Although RVH is normal for a newborn,
RVH is not normal for a 16-month old child.
View CXR image.
 This CXR shows a boot-shaped heart with an
upturned apex secondary to right ventricular
hypertrophy and a concavity of the left upper heart
border (pulmonary outflow tract hypoplasia). The aorta
may be shifted to the right (it is best seen on the right)
versus rotational artifact. The pulmonary vasculature is
decreased (hypoperfused lungs appear hyperlucent),
and the main pulmonary artery segment is small.
Hyperinflation is present, but no acute infiltrates are
seen. The CXR and EKG are consistent with the
clinical impression of Tetralogy of Fallot (TOF) with a
hypercyanotic spell, triggered by an episode of
bronchiolitis.
At this point, the patient's clinical condition
deteriorated. On 100% O2, the patient's oxygen
saturation decreased to the 40's, with increased work of
breathing and cyanosis, and decreased level of
consciousness. Midazolam and vecuronium were
administered in rapid sequence to facilitate intubation
with an endotracheal tube. What ET tube size should
be selected for this patient?
ET tube size can be estimated in several ways. A
commonly used method is the formula:
ETT = Age / 4 + 4
Thus, a two year old would need a 4.5 ETT:
4.5 = 2 / 4 + 4
This formula doesn't work well under this age.
Newborns require a 3.0 or 3.5, while an 8-month old
would probably require a 4.0 ETT. In the case of our
16-month old patient, a 4.5 ETT was used. ET tube
position was confirmed by auscultation and CXR;
however, the oxygen saturations remained in the 30's to
50's despite bag ventilation with 100% O2 through the
endotracheal tube. Continued wheezes were heard,
and albuterol aerosols were given. An ABG showed pH
7.30, pCO2 41, PO2 29, Base Excess -5.9. Another
fluid bolus was given, as well as sodium bicarbonate
and morphine, without improvement.
A cardiologist was consulted, and a stat
echocardiogram done in the E.D. showed Tetralogy of
Fallot with severe right ventricular outflow tract
obstruction. A dose of phenylephrine (alpha agonist)
was given, resulting in a rapid improvement in oxygen
saturation to 100%. Repeat ABG showed pH 7.29,
pCO2 37, pO2 132, Base Excess -8.3. Shortly
thereafter, the patient's oxygen saturation began to drift
back down into the 80's, so a phenylephrine infusion
was started, with improvement in O2 Sat to the 90's.
The patient was admitted to the Pediatric Intensive
Care Unit.
Teaching Points:
1. Tetralogy of Fallot includes four congenital heart
abnormalities: (1) a ventricular septal defect (VSD), (2)
right ventricular outflow tract obstruction, (3) right
ventricular hypertrophy, and (4) overriding of the aorta.
The right ventricular outflow tract obstruction may be in
the form of infundibular stenosis (50%), pulmonary
valve stenosis (10%), or a combination of the two
(30%). In the most severe form of the anomaly, the
pulmonary valve is atretic (10%).
2. Tetralogy of Fallot was suspected in this patient
because of cyanosis and hypoxemia out of proportion to
the degree of wheezing and respiratory distress. He
had previously been followed with the diagnosis of VSD
without confirmation by echocardiogram.
3. The possibility of foreign body aspiration should
also be considered in any child this age with wheezing
and cyanosis. In this case, the CXR findings supported
the diagnosis of TOF. If the CXR had instead shown
findings consistent with foreign body aspiration, such as
asymmetric atelectasis, consolidation, or air trapping,
bronchoscopy should be performed. Comparison of
inspiratory and expiratory films may aid in making the
diagnosis of foreign body aspiration.
4. In TOF, the large nonrestrictive VSD results in
identical systolic pressures in the right and left
ventricles. Depending on the degree of the right
ventricular outflow tract obstruction, either a left-to-right
or a right-to-left shunt is present. In acyanotic TOF,
mild pulmonary stenosis results in a left-to-right shunt.
In cyanotic TOF, more severe degrees of pulmonary
stenosis result in a right-to-left shunt. Children with the
acyanotic form of TOF gradually develop the cyanotic
form by 1-3 years due to worsening pulmonary
hypertension.
5. The classic CXR of cyanotic TOF shows a
"boot-shaped" heart caused by enlargement of the right
ventricle and concavity of the upper left heart border
(caused by hypoplasia of the main pulmonary artery
segment). Heart size is usually normal, and pulmonary
vascular markings are decreased. The CXR of
acyanotic TOF is indistinguishable from that of a small
to moderate VSD, and may show increased heart size
and increased pulmonary vascular markings because of
the left-to-right shunt.
6. Episodes of paroxysmal hypoxemia, also called
hypercyanotic or tetralogy spells ("Tet Spells") are seen
commonly in infants and children with TOF. They are
caused by lowering of the systemic vascular resistance
or increasing resistance to right ventricular pulmonary
outflow, resulting in increased right-to-left shunting at
the level of the VSD. Increased cyanosis stimulates the
respiratory center to produce hyperpnea. This in turn
results in an increase in systemic venous return,
increasing the right-to-left shunt through the VSD. This
creates a vicious cycle with worsening cyanosis. The
spells are usually self-limited, but severe spells may be
fatal.
7. Treatment of a hypercyanotic spell includes the
following:
a) Place the child in the knee-chest position. This
increases the systemic vascular resistance by
compressing the arterial circulation of the lower
extremities. This should decrease the amount of
right-to-left shunting and favor pulmonary blood flow.
b) Administer oxygen; however, realize that this has
limited benefit, since the problem is reduced pulmonary
blood flow, not the ability to deliver oxygen to the lungs.
c) Administer morphine sulfate 0.1 mg/kg IV or IM.
The benefit of morphine sulfate may be in suppressing
the respiratory center and decreasing hyperpnea.
d) Treat the metabolic acidosis with sodium
bicarbonate, 1 mEq/kg IV. This reduces the respiratory
stimulation by metabolic acidosis, and may diminish the
increase in pulmonary vascular resistance caused by
hypoxia and acidosis.
e) Administer phenylephrine 5-20 mcg/kg IV every
10-15 minutes as needed. Phenylephrine increases the
systemic vascular resistance, forcing more blood flow to
the lungs (i.e., decreasing the degree of right to left
shunting across the VSD). Our patient did not respond
to the knee-chest position, oxygen, morphine sulfate, or
sodium bicarbonate, but showed dramatic improvement
after phenylephrine administration. He ultimately
required a continuous phenylephrine infusion to
maintain adequate pulmonary blood flow to keep
oxygen saturations in the 90's. A phenylephrine drip
may be run at 0.1-0.5 mcg/kg/min, titrated to desired
effect. Phenylephrine is a potent vasoconstrictor that
will result in reduced renal and mesenteric perfusion as
well.
f) Administer propranolol, 0.1 mg/kg slow IV push.
The dose may be repeated in 15 minutes. By
decreasing cardiac contractility, propranolol may
decrease infundibular obstruction of right ventricular
outflow. Propranolol may also be given orally at 2-4
mg/kg/day PO to prevent hypercyanotic spells. When
used chronically, propranolol may also have the
beneficial effect of stabilizing peripheral vascular
reactivity. Propranolol is a beta blocker and this may
induce bronchospasm in patients prone to this.
References:
1. Neches WH and Ettedgui JA. Tetralogy of Fallot.
In Oski FA ed. Principles and Practice of Pediatrics.
Philadelphia, J.B. Lippincott Co., 1990, pp. 1402-1405.
2. Park MK. The Pediatric Cardiology Handbook.
St. Louis, Mosby-Year Book Inc., 1991, pp. 92-98.
3. van Roekens CN, Zuckerberg AL. Emergency
Management of Hypercyanotic Crisis in Tetralogy of
Fallot. Annals of Emergency Medicine
1995;25:256-258.
This CXR shows a boot-shaped heart with an
upturned apex secondary to right ventricular
hypertrophy and a concavity of the left upper heart
border (pulmonary outflow tract hypoplasia). The aorta
may be shifted to the right (it is best seen on the right)
versus rotational artifact. The pulmonary vasculature is
decreased (hypoperfused lungs appear hyperlucent),
and the main pulmonary artery segment is small.
Hyperinflation is present, but no acute infiltrates are
seen. The CXR and EKG are consistent with the
clinical impression of Tetralogy of Fallot (TOF) with a
hypercyanotic spell, triggered by an episode of
bronchiolitis.
At this point, the patient's clinical condition
deteriorated. On 100% O2, the patient's oxygen
saturation decreased to the 40's, with increased work of
breathing and cyanosis, and decreased level of
consciousness. Midazolam and vecuronium were
administered in rapid sequence to facilitate intubation
with an endotracheal tube. What ET tube size should
be selected for this patient?
ET tube size can be estimated in several ways. A
commonly used method is the formula:
ETT = Age / 4 + 4
Thus, a two year old would need a 4.5 ETT:
4.5 = 2 / 4 + 4
This formula doesn't work well under this age.
Newborns require a 3.0 or 3.5, while an 8-month old
would probably require a 4.0 ETT. In the case of our
16-month old patient, a 4.5 ETT was used. ET tube
position was confirmed by auscultation and CXR;
however, the oxygen saturations remained in the 30's to
50's despite bag ventilation with 100% O2 through the
endotracheal tube. Continued wheezes were heard,
and albuterol aerosols were given. An ABG showed pH
7.30, pCO2 41, PO2 29, Base Excess -5.9. Another
fluid bolus was given, as well as sodium bicarbonate
and morphine, without improvement.
A cardiologist was consulted, and a stat
echocardiogram done in the E.D. showed Tetralogy of
Fallot with severe right ventricular outflow tract
obstruction. A dose of phenylephrine (alpha agonist)
was given, resulting in a rapid improvement in oxygen
saturation to 100%. Repeat ABG showed pH 7.29,
pCO2 37, pO2 132, Base Excess -8.3. Shortly
thereafter, the patient's oxygen saturation began to drift
back down into the 80's, so a phenylephrine infusion
was started, with improvement in O2 Sat to the 90's.
The patient was admitted to the Pediatric Intensive
Care Unit.
Teaching Points:
1. Tetralogy of Fallot includes four congenital heart
abnormalities: (1) a ventricular septal defect (VSD), (2)
right ventricular outflow tract obstruction, (3) right
ventricular hypertrophy, and (4) overriding of the aorta.
The right ventricular outflow tract obstruction may be in
the form of infundibular stenosis (50%), pulmonary
valve stenosis (10%), or a combination of the two
(30%). In the most severe form of the anomaly, the
pulmonary valve is atretic (10%).
2. Tetralogy of Fallot was suspected in this patient
because of cyanosis and hypoxemia out of proportion to
the degree of wheezing and respiratory distress. He
had previously been followed with the diagnosis of VSD
without confirmation by echocardiogram.
3. The possibility of foreign body aspiration should
also be considered in any child this age with wheezing
and cyanosis. In this case, the CXR findings supported
the diagnosis of TOF. If the CXR had instead shown
findings consistent with foreign body aspiration, such as
asymmetric atelectasis, consolidation, or air trapping,
bronchoscopy should be performed. Comparison of
inspiratory and expiratory films may aid in making the
diagnosis of foreign body aspiration.
4. In TOF, the large nonrestrictive VSD results in
identical systolic pressures in the right and left
ventricles. Depending on the degree of the right
ventricular outflow tract obstruction, either a left-to-right
or a right-to-left shunt is present. In acyanotic TOF,
mild pulmonary stenosis results in a left-to-right shunt.
In cyanotic TOF, more severe degrees of pulmonary
stenosis result in a right-to-left shunt. Children with the
acyanotic form of TOF gradually develop the cyanotic
form by 1-3 years due to worsening pulmonary
hypertension.
5. The classic CXR of cyanotic TOF shows a
"boot-shaped" heart caused by enlargement of the right
ventricle and concavity of the upper left heart border
(caused by hypoplasia of the main pulmonary artery
segment). Heart size is usually normal, and pulmonary
vascular markings are decreased. The CXR of
acyanotic TOF is indistinguishable from that of a small
to moderate VSD, and may show increased heart size
and increased pulmonary vascular markings because of
the left-to-right shunt.
6. Episodes of paroxysmal hypoxemia, also called
hypercyanotic or tetralogy spells ("Tet Spells") are seen
commonly in infants and children with TOF. They are
caused by lowering of the systemic vascular resistance
or increasing resistance to right ventricular pulmonary
outflow, resulting in increased right-to-left shunting at
the level of the VSD. Increased cyanosis stimulates the
respiratory center to produce hyperpnea. This in turn
results in an increase in systemic venous return,
increasing the right-to-left shunt through the VSD. This
creates a vicious cycle with worsening cyanosis. The
spells are usually self-limited, but severe spells may be
fatal.
7. Treatment of a hypercyanotic spell includes the
following:
a) Place the child in the knee-chest position. This
increases the systemic vascular resistance by
compressing the arterial circulation of the lower
extremities. This should decrease the amount of
right-to-left shunting and favor pulmonary blood flow.
b) Administer oxygen; however, realize that this has
limited benefit, since the problem is reduced pulmonary
blood flow, not the ability to deliver oxygen to the lungs.
c) Administer morphine sulfate 0.1 mg/kg IV or IM.
The benefit of morphine sulfate may be in suppressing
the respiratory center and decreasing hyperpnea.
d) Treat the metabolic acidosis with sodium
bicarbonate, 1 mEq/kg IV. This reduces the respiratory
stimulation by metabolic acidosis, and may diminish the
increase in pulmonary vascular resistance caused by
hypoxia and acidosis.
e) Administer phenylephrine 5-20 mcg/kg IV every
10-15 minutes as needed. Phenylephrine increases the
systemic vascular resistance, forcing more blood flow to
the lungs (i.e., decreasing the degree of right to left
shunting across the VSD). Our patient did not respond
to the knee-chest position, oxygen, morphine sulfate, or
sodium bicarbonate, but showed dramatic improvement
after phenylephrine administration. He ultimately
required a continuous phenylephrine infusion to
maintain adequate pulmonary blood flow to keep
oxygen saturations in the 90's. A phenylephrine drip
may be run at 0.1-0.5 mcg/kg/min, titrated to desired
effect. Phenylephrine is a potent vasoconstrictor that
will result in reduced renal and mesenteric perfusion as
well.
f) Administer propranolol, 0.1 mg/kg slow IV push.
The dose may be repeated in 15 minutes. By
decreasing cardiac contractility, propranolol may
decrease infundibular obstruction of right ventricular
outflow. Propranolol may also be given orally at 2-4
mg/kg/day PO to prevent hypercyanotic spells. When
used chronically, propranolol may also have the
beneficial effect of stabilizing peripheral vascular
reactivity. Propranolol is a beta blocker and this may
induce bronchospasm in patients prone to this.
References:
1. Neches WH and Ettedgui JA. Tetralogy of Fallot.
In Oski FA ed. Principles and Practice of Pediatrics.
Philadelphia, J.B. Lippincott Co., 1990, pp. 1402-1405.
2. Park MK. The Pediatric Cardiology Handbook.
St. Louis, Mosby-Year Book Inc., 1991, pp. 92-98.
3. van Roekens CN, Zuckerberg AL. Emergency
Management of Hypercyanotic Crisis in Tetralogy of
Fallot. Annals of Emergency Medicine
1995;25:256-258.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Determine the axis of QRS in the frontal plane
(using the limb leads). Note that several leads are
isoelectric (I, AVF, and AVL). Since I and AVF are
perpendicular to each other, this represents misplaced
leads or the axis is perpendicular to both leads (ie., an
anterior or posterior axis). The cardiologist reviewing
this EKG noted the axis to be "indeterminate",
indicating that the axis of QRS is largely perpendicular
to the frontal plane. The cardiologist has re-labeled
leads V1-V3. Regardless of this change, it appears that
the axis of QRS is anterior since V1 and V2 are greatly
positive (large R waves). The large R waves in lead
V1, V2, and V3 meet voltage criteria for right ventricular
hypertrophy. Although RVH usually has a right axis in
the frontal plane (greater than 90 degrees), the right
ventricle is anterior; thus, it may have an anterior
axis as well. Although RVH is normal for a newborn,
RVH is not normal for a 16-month old child.
View CXR image.
Determine the axis of QRS in the frontal plane
(using the limb leads). Note that several leads are
isoelectric (I, AVF, and AVL). Since I and AVF are
perpendicular to each other, this represents misplaced
leads or the axis is perpendicular to both leads (ie., an
anterior or posterior axis). The cardiologist reviewing
this EKG noted the axis to be "indeterminate",
indicating that the axis of QRS is largely perpendicular
to the frontal plane. The cardiologist has re-labeled
leads V1-V3. Regardless of this change, it appears that
the axis of QRS is anterior since V1 and V2 are greatly
positive (large R waves). The large R waves in lead
V1, V2, and V3 meet voltage criteria for right ventricular
hypertrophy. Although RVH usually has a right axis in
the frontal plane (greater than 90 degrees), the right
ventricle is anterior; thus, it may have an anterior
axis as well. Although RVH is normal for a newborn,
RVH is not normal for a 16-month old child.
View CXR image.
 This CXR shows a boot-shaped heart with an
upturned apex secondary to right ventricular
hypertrophy and a concavity of the left upper heart
border (pulmonary outflow tract hypoplasia). The aorta
may be shifted to the right (it is best seen on the right)
versus rotational artifact. The pulmonary vasculature is
decreased (hypoperfused lungs appear hyperlucent),
and the main pulmonary artery segment is small.
Hyperinflation is present, but no acute infiltrates are
seen. The CXR and EKG are consistent with the
clinical impression of Tetralogy of Fallot (TOF) with a
hypercyanotic spell, triggered by an episode of
bronchiolitis.
At this point, the patient's clinical condition
deteriorated. On 100% O2, the patient's oxygen
saturation decreased to the 40's, with increased work of
breathing and cyanosis, and decreased level of
consciousness. Midazolam and vecuronium were
administered in rapid sequence to facilitate intubation
with an endotracheal tube. What ET tube size should
be selected for this patient?
ET tube size can be estimated in several ways. A
commonly used method is the formula:
ETT = Age / 4 + 4
Thus, a two year old would need a 4.5 ETT:
4.5 = 2 / 4 + 4
This formula doesn't work well under this age.
Newborns require a 3.0 or 3.5, while an 8-month old
would probably require a 4.0 ETT. In the case of our
16-month old patient, a 4.5 ETT was used. ET tube
position was confirmed by auscultation and CXR;
however, the oxygen saturations remained in the 30's to
50's despite bag ventilation with 100% O2 through the
endotracheal tube. Continued wheezes were heard,
and albuterol aerosols were given. An ABG showed pH
7.30, pCO2 41, PO2 29, Base Excess -5.9. Another
fluid bolus was given, as well as sodium bicarbonate
and morphine, without improvement.
A cardiologist was consulted, and a stat
echocardiogram done in the E.D. showed Tetralogy of
Fallot with severe right ventricular outflow tract
obstruction. A dose of phenylephrine (alpha agonist)
was given, resulting in a rapid improvement in oxygen
saturation to 100%. Repeat ABG showed pH 7.29,
pCO2 37, pO2 132, Base Excess -8.3. Shortly
thereafter, the patient's oxygen saturation began to drift
back down into the 80's, so a phenylephrine infusion
was started, with improvement in O2 Sat to the 90's.
The patient was admitted to the Pediatric Intensive
Care Unit.
Teaching Points:
1. Tetralogy of Fallot includes four congenital heart
abnormalities: (1) a ventricular septal defect (VSD), (2)
right ventricular outflow tract obstruction, (3) right
ventricular hypertrophy, and (4) overriding of the aorta.
The right ventricular outflow tract obstruction may be in
the form of infundibular stenosis (50%), pulmonary
valve stenosis (10%), or a combination of the two
(30%). In the most severe form of the anomaly, the
pulmonary valve is atretic (10%).
2. Tetralogy of Fallot was suspected in this patient
because of cyanosis and hypoxemia out of proportion to
the degree of wheezing and respiratory distress. He
had previously been followed with the diagnosis of VSD
without confirmation by echocardiogram.
3. The possibility of foreign body aspiration should
also be considered in any child this age with wheezing
and cyanosis. In this case, the CXR findings supported
the diagnosis of TOF. If the CXR had instead shown
findings consistent with foreign body aspiration, such as
asymmetric atelectasis, consolidation, or air trapping,
bronchoscopy should be performed. Comparison of
inspiratory and expiratory films may aid in making the
diagnosis of foreign body aspiration.
4. In TOF, the large nonrestrictive VSD results in
identical systolic pressures in the right and left
ventricles. Depending on the degree of the right
ventricular outflow tract obstruction, either a left-to-right
or a right-to-left shunt is present. In acyanotic TOF,
mild pulmonary stenosis results in a left-to-right shunt.
In cyanotic TOF, more severe degrees of pulmonary
stenosis result in a right-to-left shunt. Children with the
acyanotic form of TOF gradually develop the cyanotic
form by 1-3 years due to worsening pulmonary
hypertension.
5. The classic CXR of cyanotic TOF shows a
"boot-shaped" heart caused by enlargement of the right
ventricle and concavity of the upper left heart border
(caused by hypoplasia of the main pulmonary artery
segment). Heart size is usually normal, and pulmonary
vascular markings are decreased. The CXR of
acyanotic TOF is indistinguishable from that of a small
to moderate VSD, and may show increased heart size
and increased pulmonary vascular markings because of
the left-to-right shunt.
6. Episodes of paroxysmal hypoxemia, also called
hypercyanotic or tetralogy spells ("Tet Spells") are seen
commonly in infants and children with TOF. They are
caused by lowering of the systemic vascular resistance
or increasing resistance to right ventricular pulmonary
outflow, resulting in increased right-to-left shunting at
the level of the VSD. Increased cyanosis stimulates the
respiratory center to produce hyperpnea. This in turn
results in an increase in systemic venous return,
increasing the right-to-left shunt through the VSD. This
creates a vicious cycle with worsening cyanosis. The
spells are usually self-limited, but severe spells may be
fatal.
7. Treatment of a hypercyanotic spell includes the
following:
a) Place the child in the knee-chest position. This
increases the systemic vascular resistance by
compressing the arterial circulation of the lower
extremities. This should decrease the amount of
right-to-left shunting and favor pulmonary blood flow.
b) Administer oxygen; however, realize that this has
limited benefit, since the problem is reduced pulmonary
blood flow, not the ability to deliver oxygen to the lungs.
c) Administer morphine sulfate 0.1 mg/kg IV or IM.
The benefit of morphine sulfate may be in suppressing
the respiratory center and decreasing hyperpnea.
d) Treat the metabolic acidosis with sodium
bicarbonate, 1 mEq/kg IV. This reduces the respiratory
stimulation by metabolic acidosis, and may diminish the
increase in pulmonary vascular resistance caused by
hypoxia and acidosis.
e) Administer phenylephrine 5-20 mcg/kg IV every
10-15 minutes as needed. Phenylephrine increases the
systemic vascular resistance, forcing more blood flow to
the lungs (i.e., decreasing the degree of right to left
shunting across the VSD). Our patient did not respond
to the knee-chest position, oxygen, morphine sulfate, or
sodium bicarbonate, but showed dramatic improvement
after phenylephrine administration. He ultimately
required a continuous phenylephrine infusion to
maintain adequate pulmonary blood flow to keep
oxygen saturations in the 90's. A phenylephrine drip
may be run at 0.1-0.5 mcg/kg/min, titrated to desired
effect. Phenylephrine is a potent vasoconstrictor that
will result in reduced renal and mesenteric perfusion as
well.
f) Administer propranolol, 0.1 mg/kg slow IV push.
The dose may be repeated in 15 minutes. By
decreasing cardiac contractility, propranolol may
decrease infundibular obstruction of right ventricular
outflow. Propranolol may also be given orally at 2-4
mg/kg/day PO to prevent hypercyanotic spells. When
used chronically, propranolol may also have the
beneficial effect of stabilizing peripheral vascular
reactivity. Propranolol is a beta blocker and this may
induce bronchospasm in patients prone to this.
References:
1. Neches WH and Ettedgui JA. Tetralogy of Fallot.
In Oski FA ed. Principles and Practice of Pediatrics.
Philadelphia, J.B. Lippincott Co., 1990, pp. 1402-1405.
2. Park MK. The Pediatric Cardiology Handbook.
St. Louis, Mosby-Year Book Inc., 1991, pp. 92-98.
3. van Roekens CN, Zuckerberg AL. Emergency
Management of Hypercyanotic Crisis in Tetralogy of
Fallot. Annals of Emergency Medicine
1995;25:256-258.
This CXR shows a boot-shaped heart with an
upturned apex secondary to right ventricular
hypertrophy and a concavity of the left upper heart
border (pulmonary outflow tract hypoplasia). The aorta
may be shifted to the right (it is best seen on the right)
versus rotational artifact. The pulmonary vasculature is
decreased (hypoperfused lungs appear hyperlucent),
and the main pulmonary artery segment is small.
Hyperinflation is present, but no acute infiltrates are
seen. The CXR and EKG are consistent with the
clinical impression of Tetralogy of Fallot (TOF) with a
hypercyanotic spell, triggered by an episode of
bronchiolitis.
At this point, the patient's clinical condition
deteriorated. On 100% O2, the patient's oxygen
saturation decreased to the 40's, with increased work of
breathing and cyanosis, and decreased level of
consciousness. Midazolam and vecuronium were
administered in rapid sequence to facilitate intubation
with an endotracheal tube. What ET tube size should
be selected for this patient?
ET tube size can be estimated in several ways. A
commonly used method is the formula:
ETT = Age / 4 + 4
Thus, a two year old would need a 4.5 ETT:
4.5 = 2 / 4 + 4
This formula doesn't work well under this age.
Newborns require a 3.0 or 3.5, while an 8-month old
would probably require a 4.0 ETT. In the case of our
16-month old patient, a 4.5 ETT was used. ET tube
position was confirmed by auscultation and CXR;
however, the oxygen saturations remained in the 30's to
50's despite bag ventilation with 100% O2 through the
endotracheal tube. Continued wheezes were heard,
and albuterol aerosols were given. An ABG showed pH
7.30, pCO2 41, PO2 29, Base Excess -5.9. Another
fluid bolus was given, as well as sodium bicarbonate
and morphine, without improvement.
A cardiologist was consulted, and a stat
echocardiogram done in the E.D. showed Tetralogy of
Fallot with severe right ventricular outflow tract
obstruction. A dose of phenylephrine (alpha agonist)
was given, resulting in a rapid improvement in oxygen
saturation to 100%. Repeat ABG showed pH 7.29,
pCO2 37, pO2 132, Base Excess -8.3. Shortly
thereafter, the patient's oxygen saturation began to drift
back down into the 80's, so a phenylephrine infusion
was started, with improvement in O2 Sat to the 90's.
The patient was admitted to the Pediatric Intensive
Care Unit.
Teaching Points:
1. Tetralogy of Fallot includes four congenital heart
abnormalities: (1) a ventricular septal defect (VSD), (2)
right ventricular outflow tract obstruction, (3) right
ventricular hypertrophy, and (4) overriding of the aorta.
The right ventricular outflow tract obstruction may be in
the form of infundibular stenosis (50%), pulmonary
valve stenosis (10%), or a combination of the two
(30%). In the most severe form of the anomaly, the
pulmonary valve is atretic (10%).
2. Tetralogy of Fallot was suspected in this patient
because of cyanosis and hypoxemia out of proportion to
the degree of wheezing and respiratory distress. He
had previously been followed with the diagnosis of VSD
without confirmation by echocardiogram.
3. The possibility of foreign body aspiration should
also be considered in any child this age with wheezing
and cyanosis. In this case, the CXR findings supported
the diagnosis of TOF. If the CXR had instead shown
findings consistent with foreign body aspiration, such as
asymmetric atelectasis, consolidation, or air trapping,
bronchoscopy should be performed. Comparison of
inspiratory and expiratory films may aid in making the
diagnosis of foreign body aspiration.
4. In TOF, the large nonrestrictive VSD results in
identical systolic pressures in the right and left
ventricles. Depending on the degree of the right
ventricular outflow tract obstruction, either a left-to-right
or a right-to-left shunt is present. In acyanotic TOF,
mild pulmonary stenosis results in a left-to-right shunt.
In cyanotic TOF, more severe degrees of pulmonary
stenosis result in a right-to-left shunt. Children with the
acyanotic form of TOF gradually develop the cyanotic
form by 1-3 years due to worsening pulmonary
hypertension.
5. The classic CXR of cyanotic TOF shows a
"boot-shaped" heart caused by enlargement of the right
ventricle and concavity of the upper left heart border
(caused by hypoplasia of the main pulmonary artery
segment). Heart size is usually normal, and pulmonary
vascular markings are decreased. The CXR of
acyanotic TOF is indistinguishable from that of a small
to moderate VSD, and may show increased heart size
and increased pulmonary vascular markings because of
the left-to-right shunt.
6. Episodes of paroxysmal hypoxemia, also called
hypercyanotic or tetralogy spells ("Tet Spells") are seen
commonly in infants and children with TOF. They are
caused by lowering of the systemic vascular resistance
or increasing resistance to right ventricular pulmonary
outflow, resulting in increased right-to-left shunting at
the level of the VSD. Increased cyanosis stimulates the
respiratory center to produce hyperpnea. This in turn
results in an increase in systemic venous return,
increasing the right-to-left shunt through the VSD. This
creates a vicious cycle with worsening cyanosis. The
spells are usually self-limited, but severe spells may be
fatal.
7. Treatment of a hypercyanotic spell includes the
following:
a) Place the child in the knee-chest position. This
increases the systemic vascular resistance by
compressing the arterial circulation of the lower
extremities. This should decrease the amount of
right-to-left shunting and favor pulmonary blood flow.
b) Administer oxygen; however, realize that this has
limited benefit, since the problem is reduced pulmonary
blood flow, not the ability to deliver oxygen to the lungs.
c) Administer morphine sulfate 0.1 mg/kg IV or IM.
The benefit of morphine sulfate may be in suppressing
the respiratory center and decreasing hyperpnea.
d) Treat the metabolic acidosis with sodium
bicarbonate, 1 mEq/kg IV. This reduces the respiratory
stimulation by metabolic acidosis, and may diminish the
increase in pulmonary vascular resistance caused by
hypoxia and acidosis.
e) Administer phenylephrine 5-20 mcg/kg IV every
10-15 minutes as needed. Phenylephrine increases the
systemic vascular resistance, forcing more blood flow to
the lungs (i.e., decreasing the degree of right to left
shunting across the VSD). Our patient did not respond
to the knee-chest position, oxygen, morphine sulfate, or
sodium bicarbonate, but showed dramatic improvement
after phenylephrine administration. He ultimately
required a continuous phenylephrine infusion to
maintain adequate pulmonary blood flow to keep
oxygen saturations in the 90's. A phenylephrine drip
may be run at 0.1-0.5 mcg/kg/min, titrated to desired
effect. Phenylephrine is a potent vasoconstrictor that
will result in reduced renal and mesenteric perfusion as
well.
f) Administer propranolol, 0.1 mg/kg slow IV push.
The dose may be repeated in 15 minutes. By
decreasing cardiac contractility, propranolol may
decrease infundibular obstruction of right ventricular
outflow. Propranolol may also be given orally at 2-4
mg/kg/day PO to prevent hypercyanotic spells. When
used chronically, propranolol may also have the
beneficial effect of stabilizing peripheral vascular
reactivity. Propranolol is a beta blocker and this may
induce bronchospasm in patients prone to this.
References:
1. Neches WH and Ettedgui JA. Tetralogy of Fallot.
In Oski FA ed. Principles and Practice of Pediatrics.
Philadelphia, J.B. Lippincott Co., 1990, pp. 1402-1405.
2. Park MK. The Pediatric Cardiology Handbook.
St. Louis, Mosby-Year Book Inc., 1991, pp. 92-98.
3. van Roekens CN, Zuckerberg AL. Emergency
Management of Hypercyanotic Crisis in Tetralogy of
Fallot. Annals of Emergency Medicine
1995;25:256-258.