A Hand Contusion
Radiology Cases in Pediatric Emergency Medicine
Volume 1, Case 14
Alson S. Inaba, MD
Rodney B. Boychuk, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 17 year old male presents to the ED with right
wrist and hand pain two hours after falling on his
out-stretched (extended) right hand. The patient was
jogging along the sidewalk when he lost his balance,
tripped on the curb and broke his fall by landing on his
out-stretched right hand. There was no loss of
consciousness and the only area of pain was his right
wrist.
Exam: Except for some very superficial palmar
abrasions, there were no other visible signs of external
trauma over the entire right upper extremity from the
clavicle to the tips of the fingers. The shoulder and
elbow both demonstrated full range of motion without
any pain. His fingers were all pink with intact
neurovascular integrity. Upon closer examination of the
wrist, the patient complained of point tenderness in the
floor of the anatomic snuff box. This point tenderness
was exacerbated with wrist flexion, extension and radial
deviation. Because of point tenderness in this area,
radiographs were obtained to rule out a fracture.
View wrist radiographs: AP view
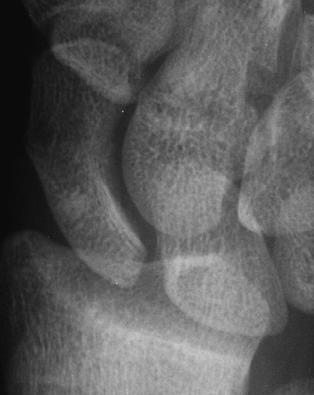
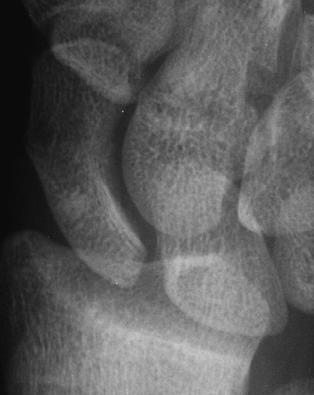
 View wrist radiographs: Oblique view
View wrist radiographs: Oblique view
 The lateral view of the wrist was not contributory so
it is not included here. A scaphoid view was also taken
because of the area of tenderness over the scaphoid.
View scaphoid radiograph.
The lateral view of the wrist was not contributory so
it is not included here. A scaphoid view was also taken
because of the area of tenderness over the scaphoid.
View scaphoid radiograph.
 Questions:
1) What is the significance of point tenderness in
the area of the scaphoid (navicular) bone?
2) How would you interpret the radiographs shown
above?
3) What are the complications of this type of injury?
4) How should these types of injuries be managed
in the ED and when should you consult an orthopedic
surgeon?
This set of radiographs were initially read by the
emergency physician as normal. However, a fracture
was still suspected and the patient was placed in a
thumb spica splint and given orthopedic referral
arrangements. A radiologist then read the radiographs
as showing a tiny fracture of the scaphoid. On the
enlarged views of the scaphoid, there is a slight
irregularity of the cortex on the lateral side. You may
have to adjust the brightness and contrast on your
monitor to appreciate this. A second radiologist
disagreed and insisted that these radiographs were
normal.
Teaching Points:
a) Point tenderness in the "anatomic snuff box"
region should always alert one to the possibility of a
scaphoid (navicular) fracture. The scaphoid bone is the
most commonly fractured carpal bone. These types of
fractures are most commonly seen in patients between
15 and 35 years of age as a result of a forceful
hyperextension type injury to the wrist.
View another example.
Questions:
1) What is the significance of point tenderness in
the area of the scaphoid (navicular) bone?
2) How would you interpret the radiographs shown
above?
3) What are the complications of this type of injury?
4) How should these types of injuries be managed
in the ED and when should you consult an orthopedic
surgeon?
This set of radiographs were initially read by the
emergency physician as normal. However, a fracture
was still suspected and the patient was placed in a
thumb spica splint and given orthopedic referral
arrangements. A radiologist then read the radiographs
as showing a tiny fracture of the scaphoid. On the
enlarged views of the scaphoid, there is a slight
irregularity of the cortex on the lateral side. You may
have to adjust the brightness and contrast on your
monitor to appreciate this. A second radiologist
disagreed and insisted that these radiographs were
normal.
Teaching Points:
a) Point tenderness in the "anatomic snuff box"
region should always alert one to the possibility of a
scaphoid (navicular) fracture. The scaphoid bone is the
most commonly fractured carpal bone. These types of
fractures are most commonly seen in patients between
15 and 35 years of age as a result of a forceful
hyperextension type injury to the wrist.
View another example.
 This patient complained of distal forearm pain. The
scaphoid region was not specifically examined. This
pitfall must be avoided. A forearm film which included
the wrist was obtained. A distal radius fracture and an
ulnar styloid fracture were noted. At the very top of the
film, where it ends, a fracture through the scaphoid was
noted. Patients may not complain of pain exactly over
the fracture site, especially when there are fractures
elsewhere. However, examination for the location(s) of
point tenderness will usually improve the clinician's
ability to locate the site of injury.
View another example.
This patient complained of distal forearm pain. The
scaphoid region was not specifically examined. This
pitfall must be avoided. A forearm film which included
the wrist was obtained. A distal radius fracture and an
ulnar styloid fracture were noted. At the very top of the
film, where it ends, a fracture through the scaphoid was
noted. Patients may not complain of pain exactly over
the fracture site, especially when there are fractures
elsewhere. However, examination for the location(s) of
point tenderness will usually improve the clinician's
ability to locate the site of injury.
View another example.
 This radiograph shows another scaphoid fracture.
However even in the absence of such a radiographically
evident fracture, point tenderness over the scaphoid
warrants the same treatment.
View the anatomic snuff box.
This radiograph shows another scaphoid fracture.
However even in the absence of such a radiographically
evident fracture, point tenderness over the scaphoid
warrants the same treatment.
View the anatomic snuff box.
 The arrow points to the floor of the anatomic snuff
box. The scaphoid bone forms the floor of the anatomic
snuff box. Tenderness in the area should raise the
suspicion of a scaphoid fracture.
b) The blood supply to the scaphoid penetrates
the cortex at both the distal aspect (on the dorsal
aspect near the scaphoid turbercle) and the waist
(middle third of the scaphoid). Because of this tenuous
blood supply, there is no direct blood supply to the
proximal third of the scaphoid. Therefore, scaphoid
fractures (even if properly diagnosed and treated) have
a tendency for dreaded complications, such as
avascular necrosis of the proximal third and non-union.
In general, the more proximal the fracture, the greater
the likelihood of avascular necrosis.
c) Although adults are more likely to present with
fractures involving the middle third or proximal aspect of
the scaphoid, children have a higher incidence of
fractures involving the distal third of the scaphoid.
d) If one is clinically suspicious of a scaphoid
fracture, always be sure to obtain isolated scaphoid
views in addition to the standard AP, lateral and oblique
views of the wrist. Even if there is no obvious
radiographic evidence of a scaphoid fracture, all
patients with point tenderness over the anatomic snuff
box region should be properly immobilized in the ED
and referred to an orthopedist for further evaluation and
management.
e) Proper immobilization of a scaphoid fracture
should prevent wrist flexion/extension, radial wrist
deviation and any movement of the thumb metacarpal.
Therefore a simple volar wrist splint would NOT be
considered proper immobilization for a scaphoid
fracture. A more adequate immobilization technique
would be to apply a thumb spica/radial gutter splint
(which could also be combined with a volar wrist splint).
View thumb spica/radial gutter splint.
The arrow points to the floor of the anatomic snuff
box. The scaphoid bone forms the floor of the anatomic
snuff box. Tenderness in the area should raise the
suspicion of a scaphoid fracture.
b) The blood supply to the scaphoid penetrates
the cortex at both the distal aspect (on the dorsal
aspect near the scaphoid turbercle) and the waist
(middle third of the scaphoid). Because of this tenuous
blood supply, there is no direct blood supply to the
proximal third of the scaphoid. Therefore, scaphoid
fractures (even if properly diagnosed and treated) have
a tendency for dreaded complications, such as
avascular necrosis of the proximal third and non-union.
In general, the more proximal the fracture, the greater
the likelihood of avascular necrosis.
c) Although adults are more likely to present with
fractures involving the middle third or proximal aspect of
the scaphoid, children have a higher incidence of
fractures involving the distal third of the scaphoid.
d) If one is clinically suspicious of a scaphoid
fracture, always be sure to obtain isolated scaphoid
views in addition to the standard AP, lateral and oblique
views of the wrist. Even if there is no obvious
radiographic evidence of a scaphoid fracture, all
patients with point tenderness over the anatomic snuff
box region should be properly immobilized in the ED
and referred to an orthopedist for further evaluation and
management.
e) Proper immobilization of a scaphoid fracture
should prevent wrist flexion/extension, radial wrist
deviation and any movement of the thumb metacarpal.
Therefore a simple volar wrist splint would NOT be
considered proper immobilization for a scaphoid
fracture. A more adequate immobilization technique
would be to apply a thumb spica/radial gutter splint
(which could also be combined with a volar wrist splint).
View thumb spica/radial gutter splint.
 Only the radial gutter and thumb immobilizing
portion of the splint is shown here without the overlying
elastic wrap. The thumb is immobilized to prevent wrist
ab/ad-duction and first metacarpal movement. A volar
splint can be added to this.
f) Definitive treatment by an orthopedic surgeon
usually involves a thumb spica cast for 6-12 weeks.
References
1. Simon RR, Koenigsknecht SJ: Emergency
Orthopedics: The Extremities (second edition).
Appleton & Lange, pp. 81-84, 1987.
2. Letts RM: Management of Pediatric Fractures.
Churchill Livingston, pp. 389-396, 1994.
3. Etzwiler LS. Hand and Wrist Injuries. In:
Barkin R (ed). Pediatric Emergency Medicine Concepts
and Clinical Practice. Chicago, Mosby Year Book,
1992, p. 332.
Only the radial gutter and thumb immobilizing
portion of the splint is shown here without the overlying
elastic wrap. The thumb is immobilized to prevent wrist
ab/ad-duction and first metacarpal movement. A volar
splint can be added to this.
f) Definitive treatment by an orthopedic surgeon
usually involves a thumb spica cast for 6-12 weeks.
References
1. Simon RR, Koenigsknecht SJ: Emergency
Orthopedics: The Extremities (second edition).
Appleton & Lange, pp. 81-84, 1987.
2. Letts RM: Management of Pediatric Fractures.
Churchill Livingston, pp. 389-396, 1994.
3. Etzwiler LS. Hand and Wrist Injuries. In:
Barkin R (ed). Pediatric Emergency Medicine Concepts
and Clinical Practice. Chicago, Mosby Year Book,
1992, p. 332.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 View wrist radiographs: Oblique view
View wrist radiographs: Oblique view
 The lateral view of the wrist was not contributory so
it is not included here. A scaphoid view was also taken
because of the area of tenderness over the scaphoid.
View scaphoid radiograph.
The lateral view of the wrist was not contributory so
it is not included here. A scaphoid view was also taken
because of the area of tenderness over the scaphoid.
View scaphoid radiograph.
 Questions:
1) What is the significance of point tenderness in
the area of the scaphoid (navicular) bone?
2) How would you interpret the radiographs shown
above?
3) What are the complications of this type of injury?
4) How should these types of injuries be managed
in the ED and when should you consult an orthopedic
surgeon?
This set of radiographs were initially read by the
emergency physician as normal. However, a fracture
was still suspected and the patient was placed in a
thumb spica splint and given orthopedic referral
arrangements. A radiologist then read the radiographs
as showing a tiny fracture of the scaphoid. On the
enlarged views of the scaphoid, there is a slight
irregularity of the cortex on the lateral side. You may
have to adjust the brightness and contrast on your
monitor to appreciate this. A second radiologist
disagreed and insisted that these radiographs were
normal.
Teaching Points:
a) Point tenderness in the "anatomic snuff box"
region should always alert one to the possibility of a
scaphoid (navicular) fracture. The scaphoid bone is the
most commonly fractured carpal bone. These types of
fractures are most commonly seen in patients between
15 and 35 years of age as a result of a forceful
hyperextension type injury to the wrist.
View another example.
Questions:
1) What is the significance of point tenderness in
the area of the scaphoid (navicular) bone?
2) How would you interpret the radiographs shown
above?
3) What are the complications of this type of injury?
4) How should these types of injuries be managed
in the ED and when should you consult an orthopedic
surgeon?
This set of radiographs were initially read by the
emergency physician as normal. However, a fracture
was still suspected and the patient was placed in a
thumb spica splint and given orthopedic referral
arrangements. A radiologist then read the radiographs
as showing a tiny fracture of the scaphoid. On the
enlarged views of the scaphoid, there is a slight
irregularity of the cortex on the lateral side. You may
have to adjust the brightness and contrast on your
monitor to appreciate this. A second radiologist
disagreed and insisted that these radiographs were
normal.
Teaching Points:
a) Point tenderness in the "anatomic snuff box"
region should always alert one to the possibility of a
scaphoid (navicular) fracture. The scaphoid bone is the
most commonly fractured carpal bone. These types of
fractures are most commonly seen in patients between
15 and 35 years of age as a result of a forceful
hyperextension type injury to the wrist.
View another example.
 This patient complained of distal forearm pain. The
scaphoid region was not specifically examined. This
pitfall must be avoided. A forearm film which included
the wrist was obtained. A distal radius fracture and an
ulnar styloid fracture were noted. At the very top of the
film, where it ends, a fracture through the scaphoid was
noted. Patients may not complain of pain exactly over
the fracture site, especially when there are fractures
elsewhere. However, examination for the location(s) of
point tenderness will usually improve the clinician's
ability to locate the site of injury.
View another example.
This patient complained of distal forearm pain. The
scaphoid region was not specifically examined. This
pitfall must be avoided. A forearm film which included
the wrist was obtained. A distal radius fracture and an
ulnar styloid fracture were noted. At the very top of the
film, where it ends, a fracture through the scaphoid was
noted. Patients may not complain of pain exactly over
the fracture site, especially when there are fractures
elsewhere. However, examination for the location(s) of
point tenderness will usually improve the clinician's
ability to locate the site of injury.
View another example.
 This radiograph shows another scaphoid fracture.
However even in the absence of such a radiographically
evident fracture, point tenderness over the scaphoid
warrants the same treatment.
View the anatomic snuff box.
This radiograph shows another scaphoid fracture.
However even in the absence of such a radiographically
evident fracture, point tenderness over the scaphoid
warrants the same treatment.
View the anatomic snuff box.
 The arrow points to the floor of the anatomic snuff
box. The scaphoid bone forms the floor of the anatomic
snuff box. Tenderness in the area should raise the
suspicion of a scaphoid fracture.
b) The blood supply to the scaphoid penetrates
the cortex at both the distal aspect (on the dorsal
aspect near the scaphoid turbercle) and the waist
(middle third of the scaphoid). Because of this tenuous
blood supply, there is no direct blood supply to the
proximal third of the scaphoid. Therefore, scaphoid
fractures (even if properly diagnosed and treated) have
a tendency for dreaded complications, such as
avascular necrosis of the proximal third and non-union.
In general, the more proximal the fracture, the greater
the likelihood of avascular necrosis.
c) Although adults are more likely to present with
fractures involving the middle third or proximal aspect of
the scaphoid, children have a higher incidence of
fractures involving the distal third of the scaphoid.
d) If one is clinically suspicious of a scaphoid
fracture, always be sure to obtain isolated scaphoid
views in addition to the standard AP, lateral and oblique
views of the wrist. Even if there is no obvious
radiographic evidence of a scaphoid fracture, all
patients with point tenderness over the anatomic snuff
box region should be properly immobilized in the ED
and referred to an orthopedist for further evaluation and
management.
e) Proper immobilization of a scaphoid fracture
should prevent wrist flexion/extension, radial wrist
deviation and any movement of the thumb metacarpal.
Therefore a simple volar wrist splint would NOT be
considered proper immobilization for a scaphoid
fracture. A more adequate immobilization technique
would be to apply a thumb spica/radial gutter splint
(which could also be combined with a volar wrist splint).
View thumb spica/radial gutter splint.
The arrow points to the floor of the anatomic snuff
box. The scaphoid bone forms the floor of the anatomic
snuff box. Tenderness in the area should raise the
suspicion of a scaphoid fracture.
b) The blood supply to the scaphoid penetrates
the cortex at both the distal aspect (on the dorsal
aspect near the scaphoid turbercle) and the waist
(middle third of the scaphoid). Because of this tenuous
blood supply, there is no direct blood supply to the
proximal third of the scaphoid. Therefore, scaphoid
fractures (even if properly diagnosed and treated) have
a tendency for dreaded complications, such as
avascular necrosis of the proximal third and non-union.
In general, the more proximal the fracture, the greater
the likelihood of avascular necrosis.
c) Although adults are more likely to present with
fractures involving the middle third or proximal aspect of
the scaphoid, children have a higher incidence of
fractures involving the distal third of the scaphoid.
d) If one is clinically suspicious of a scaphoid
fracture, always be sure to obtain isolated scaphoid
views in addition to the standard AP, lateral and oblique
views of the wrist. Even if there is no obvious
radiographic evidence of a scaphoid fracture, all
patients with point tenderness over the anatomic snuff
box region should be properly immobilized in the ED
and referred to an orthopedist for further evaluation and
management.
e) Proper immobilization of a scaphoid fracture
should prevent wrist flexion/extension, radial wrist
deviation and any movement of the thumb metacarpal.
Therefore a simple volar wrist splint would NOT be
considered proper immobilization for a scaphoid
fracture. A more adequate immobilization technique
would be to apply a thumb spica/radial gutter splint
(which could also be combined with a volar wrist splint).
View thumb spica/radial gutter splint.
 Only the radial gutter and thumb immobilizing
portion of the splint is shown here without the overlying
elastic wrap. The thumb is immobilized to prevent wrist
ab/ad-duction and first metacarpal movement. A volar
splint can be added to this.
f) Definitive treatment by an orthopedic surgeon
usually involves a thumb spica cast for 6-12 weeks.
References
1. Simon RR, Koenigsknecht SJ: Emergency
Orthopedics: The Extremities (second edition).
Appleton & Lange, pp. 81-84, 1987.
2. Letts RM: Management of Pediatric Fractures.
Churchill Livingston, pp. 389-396, 1994.
3. Etzwiler LS. Hand and Wrist Injuries. In:
Barkin R (ed). Pediatric Emergency Medicine Concepts
and Clinical Practice. Chicago, Mosby Year Book,
1992, p. 332.
Only the radial gutter and thumb immobilizing
portion of the splint is shown here without the overlying
elastic wrap. The thumb is immobilized to prevent wrist
ab/ad-duction and first metacarpal movement. A volar
splint can be added to this.
f) Definitive treatment by an orthopedic surgeon
usually involves a thumb spica cast for 6-12 weeks.
References
1. Simon RR, Koenigsknecht SJ: Emergency
Orthopedics: The Extremities (second edition).
Appleton & Lange, pp. 81-84, 1987.
2. Letts RM: Management of Pediatric Fractures.
Churchill Livingston, pp. 389-396, 1994.
3. Etzwiler LS. Hand and Wrist Injuries. In:
Barkin R (ed). Pediatric Emergency Medicine Concepts
and Clinical Practice. Chicago, Mosby Year Book,
1992, p. 332.