Respiratory Distress - That's a Tension Pneumothorax Isn't It ?
Radiology Cases in Pediatric Emergency Medicine
Volume 1, Case 9
Linda M. Rosen, M.D.
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A two and one-half week old male infant presents
with a history of distressed noisy breathing for several
hours, progressively worsening with periods of apnea
and cyanosis. He had appeared well all day at the
baby-sitter's until one hour after his last feeding when
he was found to have the symptoms of respiratory
distress. He had no history of fever, URI symptoms,
vomiting, or diarrhea. No possible exposure to toxins or
foreign bodies could be found. Birth history was that of
a full term, NSVD, 7lb. 8oz. born to a 23 y/o G3P2
mother without sepsis risk factors. He seemed to be
doing well since discharge but had been noted by his
parents to have "funny breathing" since birth. This was
described as periodic rapid breathing with "deep caving"
in of his anterior chest. It did not cause cyanosis, nor
did it interfere with feeding. Weight gain since birth has
been appropriate.
Exam VS T36.7, P160, R60, BP 100/70. Oxygen
saturation 86% in room air. He was alert and anxious,
with obvious tachypnea and retractions. Skin color was
intermittently dusky until oxygen was administered and
then remained pink (oxygen saturation 96-100%).
Head atraumatic. No signs of URI. Neck supple.
Suprasternal, intercostal, and subcostal retractions
present. Breath sounds are faint throughout the chest,
without auscultatory rales, wheezes, or stridor heard.
Heart sounds are distant, and no murmur is heard.
Pulses are strong and regular. Capillary refill is brisk.
There are no rashes. Abdominal, neurologic, and
musculoskeletal exams are unremarkable.
A CBC with differential, blood culture, electrolytes,
glucose, UA and CXR are obtained. Room air ABG:
pH 7.33, pCO2 46, pO2 43 in room air. On oxygen by
mask, his pO2 increased to 150. A chest radiograph
is obtained.
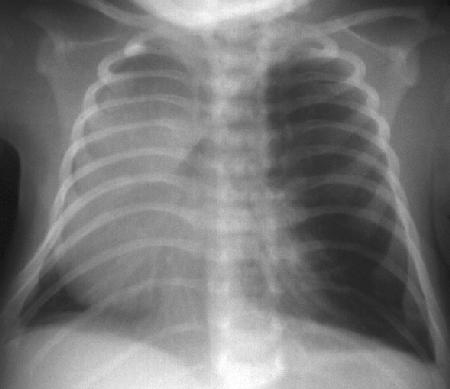
View CXR PA view.
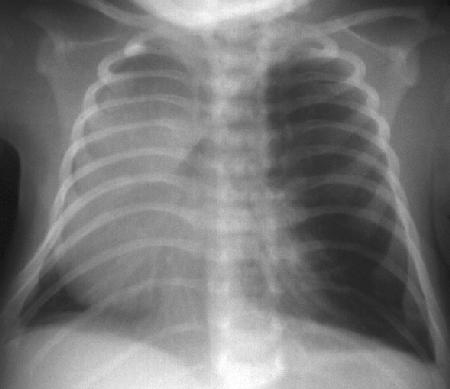
 View CXR lateral view.
View CXR lateral view.
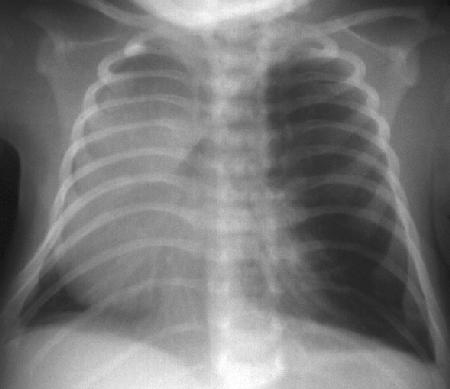
 This CXR shows hyperlucency of the left chest with
a mediastinal/cardiac shift to the right.
Management Questions:
This looks like left tension pneumothorax. Should
you perform an emergency needle thoracostomy?
Where would you do it in a 2 1/2 week old?
Before needling the chest (2nd intercostal space,
midclavicular line with an 18 or 20G catheter over the
needle) review the evidence for a tension pneumothorax.
This infant has respiratory distress with hypoxia.
Breath sounds were described as faint throughout the
chest rather than unequal. Is this consistent with a
tension pneumothorax?
Yes, infants with tension pneumothorax rarely have
unequal breath sounds. The intrathoracic volume of the
infant's chest is so small and the mediastinum is so
mobile that decreased ventilation due to free air
compressing both lungs usually results in distant or faint
breath sounds and decreased chest movement
bilaterally, rather than the differential findings between
the two sides seen in adults.
This infant's circulation does not appear
compromised clinically. The patient was alert with good
pulses and capillary refill. Is this consistent with tension
pneumothorax?
No, the hallmark of tension pneumothorax is
persistent hypoxia (despite supplemental oxygen) with
circulatory compromise (hypotension and/or
bradycardia). The fact that this patient did not have
impaired perfusion should make you refrain from
needling the chest and examine the CXR more carefully.
Re-examine the CXR.
This CXR shows hyperlucency of the left chest with
a mediastinal/cardiac shift to the right.
Management Questions:
This looks like left tension pneumothorax. Should
you perform an emergency needle thoracostomy?
Where would you do it in a 2 1/2 week old?
Before needling the chest (2nd intercostal space,
midclavicular line with an 18 or 20G catheter over the
needle) review the evidence for a tension pneumothorax.
This infant has respiratory distress with hypoxia.
Breath sounds were described as faint throughout the
chest rather than unequal. Is this consistent with a
tension pneumothorax?
Yes, infants with tension pneumothorax rarely have
unequal breath sounds. The intrathoracic volume of the
infant's chest is so small and the mediastinum is so
mobile that decreased ventilation due to free air
compressing both lungs usually results in distant or faint
breath sounds and decreased chest movement
bilaterally, rather than the differential findings between
the two sides seen in adults.
This infant's circulation does not appear
compromised clinically. The patient was alert with good
pulses and capillary refill. Is this consistent with tension
pneumothorax?
No, the hallmark of tension pneumothorax is
persistent hypoxia (despite supplemental oxygen) with
circulatory compromise (hypotension and/or
bradycardia). The fact that this patient did not have
impaired perfusion should make you refrain from
needling the chest and examine the CXR more carefully.
Re-examine the CXR.
 What at first appears to be a tension pneumothorax
may instead be severe emphysema of one or more
lobes of the lung. Every attempt should be made to
visualize lung markings and the lung edge within the
hyperlucent space. Remember that lung markings
may be very faint because the blood vessels are spread
out. Additionally, there may be reflex hypoxic
vasoconstriction as an attempt to match VQ. Carefully
examining the CXR using a hot light may prevent you
from mistakenly needling the chest and causing a
severe complication. There are indeed lung markings
throughout the left chest (These are evident on the
original film, but it was very difficult to reproduce this on
the scanned image). You decide to intubate the patient
and transfer to the ICU, but the patient's condition
worsens after intubation. What can you do?
If this patient's emphysema becomes life-threatening
(which may happen rapidly if positive pressure is
applied) the only treatment would be a lateral
thoracotomy to allow the lung to herniate out of the
chest. When you call the surgeon, he/she asks if you
are sure this is not hypoplasia of the right lung or
a diaphragmatic hernia. How do you support the
diagnosis of emphysema on CXR?
There are several parameters to assess in order to
answer this question. Before anything else, it is
essential to evaluate the CXR for the presence of any
rotation. A rotated chest film can both mimic and
obscure a mediastinal shift. Evaluation of the clavicles
is one recommended method, but is often confounded
by irregular positioning of both clavicles. Another useful
method is to evaluate the horizontal length of the ribs at
the midchest level measuring from the lateral chest to
the center of the spine on either side. If one side is
longer, the patient is rotated to that side and all
structures will appear to be falsely shifted to the same
side.
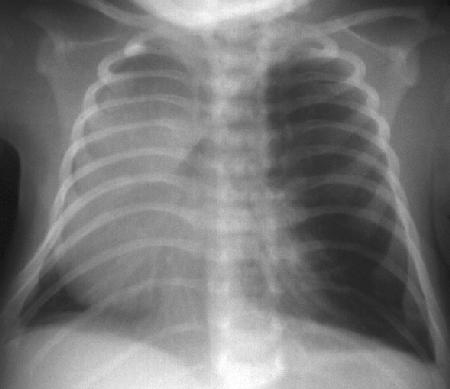
View rotated CXR.
What at first appears to be a tension pneumothorax
may instead be severe emphysema of one or more
lobes of the lung. Every attempt should be made to
visualize lung markings and the lung edge within the
hyperlucent space. Remember that lung markings
may be very faint because the blood vessels are spread
out. Additionally, there may be reflex hypoxic
vasoconstriction as an attempt to match VQ. Carefully
examining the CXR using a hot light may prevent you
from mistakenly needling the chest and causing a
severe complication. There are indeed lung markings
throughout the left chest (These are evident on the
original film, but it was very difficult to reproduce this on
the scanned image). You decide to intubate the patient
and transfer to the ICU, but the patient's condition
worsens after intubation. What can you do?
If this patient's emphysema becomes life-threatening
(which may happen rapidly if positive pressure is
applied) the only treatment would be a lateral
thoracotomy to allow the lung to herniate out of the
chest. When you call the surgeon, he/she asks if you
are sure this is not hypoplasia of the right lung or
a diaphragmatic hernia. How do you support the
diagnosis of emphysema on CXR?
There are several parameters to assess in order to
answer this question. Before anything else, it is
essential to evaluate the CXR for the presence of any
rotation. A rotated chest film can both mimic and
obscure a mediastinal shift. Evaluation of the clavicles
is one recommended method, but is often confounded
by irregular positioning of both clavicles. Another useful
method is to evaluate the horizontal length of the ribs at
the midchest level measuring from the lateral chest to
the center of the spine on either side. If one side is
longer, the patient is rotated to that side and all
structures will appear to be falsely shifted to the same
side.
View rotated CXR.
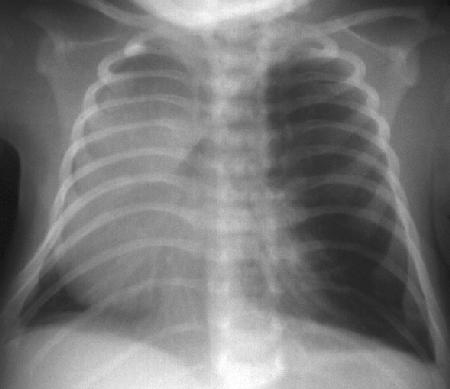
 This neonatal CXR is rotated, as can be determined
by looking at the location of the proximal clavicles and
the non-symmetry of the rib origins. This gives the
CXR the appearance of left sided hyperexpansion with
the heart pushed over to the right; however, this
appearance is purely due to rotational artifact.
Once the degree, if any, of rotation has been
determined, several other areas should be evaluated.
The bony thorax may show increased space between
the ribs on one side, indicative of emphysema or
pneumothorax. The diaphragms should be evaluated
for position and evidence of compression or elevation.
A flattened (compressed) hemidiaphragm implies
emphysema of an adjacent lobe or tension
pneumothorax. An elevated hemidiaphragm implies
volume loss in that hemithorax due to atelectasis,
hypoplasia or a diaphragmatic hernia. A decubitus film
can demonstrate failure of the emphysematous lobe to
deflate when placed down. Fluid in the hemithorax will
displace the heart, but would appear radiopaque.
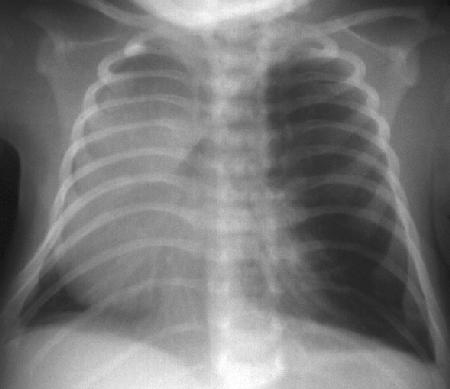
View patient's CXR again.
This neonatal CXR is rotated, as can be determined
by looking at the location of the proximal clavicles and
the non-symmetry of the rib origins. This gives the
CXR the appearance of left sided hyperexpansion with
the heart pushed over to the right; however, this
appearance is purely due to rotational artifact.
Once the degree, if any, of rotation has been
determined, several other areas should be evaluated.
The bony thorax may show increased space between
the ribs on one side, indicative of emphysema or
pneumothorax. The diaphragms should be evaluated
for position and evidence of compression or elevation.
A flattened (compressed) hemidiaphragm implies
emphysema of an adjacent lobe or tension
pneumothorax. An elevated hemidiaphragm implies
volume loss in that hemithorax due to atelectasis,
hypoplasia or a diaphragmatic hernia. A decubitus film
can demonstrate failure of the emphysematous lobe to
deflate when placed down. Fluid in the hemithorax will
displace the heart, but would appear radiopaque.
View patient's CXR again.
 Our patient's CXR shows:
1. Hyperexpanded left "lung" (actually the left upper
lobe) that herniates into the right chest.
2. Spreading of ribs of the left chest.
3. Shift of the mediastinum to the right.
4. Compression of the left hemidiaphragm.
5. Left lower lobe atelectasis (It is so small, that you
can hardly see it. It is largely obscured.) visible in the
left inferior medial chest.
6. Normal position of the right hemidiaphragm.
7. No infiltrates or fluid.
8. All these findings are consistent with emphysema
of the left upper lobe.
Discussion
An important aspect of pediatric emergency care is
to be aware of congenital anomalies and the manner
and timing with which they present. The differential
diagnosis of any acute medical presentation in the first
few months of life must include congenital problems.
Within the first weeks of life, respiratory and cardiac
problems often present precipitously.
This patient had congenital lobar emphysema of the
left upper lobe and was also found to have a patent
ductus arteriosus. The history suggests mild symptoms
since birth with acute deterioration. At lobectomy, the
left upper lobe bronchus was noted to have
abnormalities of the cartilage structures. The bronchus
was collapsed with an intraluminal mucous plug.
Emphysema may be caused by cartilaginous
malformation, intrinsic obstruction, or extrinsic
compression. This condition is most common in the
upper lobes and associated in 10% of cases with
congenital heart defects, most commonly patent ductus
arteriosus. Most cases present with respiratory distress
within the first 4 months of life and may eventually
require resection. Occasionally, asymptomatic cases
are found fortuitously on chest radiographs in later
years. Evaluation for coexisting congenital anomalies
may be made through non-invasive tests such as
echocardiography, CT, MRI, and ventilation-perfusion
lung scan.
Additional Teaching Points: Be Aware of . . .
Whenever regional emphysema is present in the
lung, suspicion of a foreign body should be very high.
The young age of our patient made this unlikely but in
the high-risk age group, approximately 5 months to 5
years of age, this diagnosis must be pursued even in
the face of a negative history. Often bronchoscopy is
needed to make the diagnosis and alleviate the
condition. Also, think of a foreign body when faced with
cases of recurrent wheezing or pneumonia (See Case
8 of Volume 1, Foreign Body Aspiration in a Child).
If this infant had a true tension pneumothorax,
staphylococcal pneumonia should be highly suspected.
It is most common in the first six months of life and
often has an extremely rapid onset with fever,
tachypnea, and grunting. Commonly, endobronchial
infection ruptures through to the pleural space, creating
a bronchopleural fistula early in the course of disease,
leading to life-threatening pneumothorax and/or
empyema. This requires urgent placement of a chest
tube, along with appropriate antibiotics and treatment
for septic shock. Staphylococcal pneumonia develops
rapidly and initial CXR findings may show no evident
infiltrate or only a smal amount of pleural fluid.
References
Gerbeaux J, Couvreur J, Tournier G. Pediatric
Respiratory Disease, second edition. New York, J.
Wiley and Sons, 1982, pp. 217-223.
Markowitz RI, Mercurio MR, Vahjen GA, Gross I,
Touloukian RT. Congenital Lobar Emphysema.
Clinical Pediatrics 1989;28(1):19-23.
Scarpeli EM, Auld P, Goldman HS. Pulmonary
Disease of the Fetus, Newborn, and Child.
Philadelphia, Lea & Febiger, 1978, pp. 194-196.
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S. Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams &
Wilkins, 1993, pp. 1336-1362.
Our patient's CXR shows:
1. Hyperexpanded left "lung" (actually the left upper
lobe) that herniates into the right chest.
2. Spreading of ribs of the left chest.
3. Shift of the mediastinum to the right.
4. Compression of the left hemidiaphragm.
5. Left lower lobe atelectasis (It is so small, that you
can hardly see it. It is largely obscured.) visible in the
left inferior medial chest.
6. Normal position of the right hemidiaphragm.
7. No infiltrates or fluid.
8. All these findings are consistent with emphysema
of the left upper lobe.
Discussion
An important aspect of pediatric emergency care is
to be aware of congenital anomalies and the manner
and timing with which they present. The differential
diagnosis of any acute medical presentation in the first
few months of life must include congenital problems.
Within the first weeks of life, respiratory and cardiac
problems often present precipitously.
This patient had congenital lobar emphysema of the
left upper lobe and was also found to have a patent
ductus arteriosus. The history suggests mild symptoms
since birth with acute deterioration. At lobectomy, the
left upper lobe bronchus was noted to have
abnormalities of the cartilage structures. The bronchus
was collapsed with an intraluminal mucous plug.
Emphysema may be caused by cartilaginous
malformation, intrinsic obstruction, or extrinsic
compression. This condition is most common in the
upper lobes and associated in 10% of cases with
congenital heart defects, most commonly patent ductus
arteriosus. Most cases present with respiratory distress
within the first 4 months of life and may eventually
require resection. Occasionally, asymptomatic cases
are found fortuitously on chest radiographs in later
years. Evaluation for coexisting congenital anomalies
may be made through non-invasive tests such as
echocardiography, CT, MRI, and ventilation-perfusion
lung scan.
Additional Teaching Points: Be Aware of . . .
Whenever regional emphysema is present in the
lung, suspicion of a foreign body should be very high.
The young age of our patient made this unlikely but in
the high-risk age group, approximately 5 months to 5
years of age, this diagnosis must be pursued even in
the face of a negative history. Often bronchoscopy is
needed to make the diagnosis and alleviate the
condition. Also, think of a foreign body when faced with
cases of recurrent wheezing or pneumonia (See Case
8 of Volume 1, Foreign Body Aspiration in a Child).
If this infant had a true tension pneumothorax,
staphylococcal pneumonia should be highly suspected.
It is most common in the first six months of life and
often has an extremely rapid onset with fever,
tachypnea, and grunting. Commonly, endobronchial
infection ruptures through to the pleural space, creating
a bronchopleural fistula early in the course of disease,
leading to life-threatening pneumothorax and/or
empyema. This requires urgent placement of a chest
tube, along with appropriate antibiotics and treatment
for septic shock. Staphylococcal pneumonia develops
rapidly and initial CXR findings may show no evident
infiltrate or only a smal amount of pleural fluid.
References
Gerbeaux J, Couvreur J, Tournier G. Pediatric
Respiratory Disease, second edition. New York, J.
Wiley and Sons, 1982, pp. 217-223.
Markowitz RI, Mercurio MR, Vahjen GA, Gross I,
Touloukian RT. Congenital Lobar Emphysema.
Clinical Pediatrics 1989;28(1):19-23.
Scarpeli EM, Auld P, Goldman HS. Pulmonary
Disease of the Fetus, Newborn, and Child.
Philadelphia, Lea & Febiger, 1978, pp. 194-196.
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S. Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams &
Wilkins, 1993, pp. 1336-1362.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 View CXR lateral view.
View CXR lateral view.
 This CXR shows hyperlucency of the left chest with
a mediastinal/cardiac shift to the right.
Management Questions:
This looks like left tension pneumothorax. Should
you perform an emergency needle thoracostomy?
Where would you do it in a 2 1/2 week old?
Before needling the chest (2nd intercostal space,
midclavicular line with an 18 or 20G catheter over the
needle) review the evidence for a tension pneumothorax.
This infant has respiratory distress with hypoxia.
Breath sounds were described as faint throughout the
chest rather than unequal. Is this consistent with a
tension pneumothorax?
Yes, infants with tension pneumothorax rarely have
unequal breath sounds. The intrathoracic volume of the
infant's chest is so small and the mediastinum is so
mobile that decreased ventilation due to free air
compressing both lungs usually results in distant or faint
breath sounds and decreased chest movement
bilaterally, rather than the differential findings between
the two sides seen in adults.
This infant's circulation does not appear
compromised clinically. The patient was alert with good
pulses and capillary refill. Is this consistent with tension
pneumothorax?
No, the hallmark of tension pneumothorax is
persistent hypoxia (despite supplemental oxygen) with
circulatory compromise (hypotension and/or
bradycardia). The fact that this patient did not have
impaired perfusion should make you refrain from
needling the chest and examine the CXR more carefully.
Re-examine the CXR.
This CXR shows hyperlucency of the left chest with
a mediastinal/cardiac shift to the right.
Management Questions:
This looks like left tension pneumothorax. Should
you perform an emergency needle thoracostomy?
Where would you do it in a 2 1/2 week old?
Before needling the chest (2nd intercostal space,
midclavicular line with an 18 or 20G catheter over the
needle) review the evidence for a tension pneumothorax.
This infant has respiratory distress with hypoxia.
Breath sounds were described as faint throughout the
chest rather than unequal. Is this consistent with a
tension pneumothorax?
Yes, infants with tension pneumothorax rarely have
unequal breath sounds. The intrathoracic volume of the
infant's chest is so small and the mediastinum is so
mobile that decreased ventilation due to free air
compressing both lungs usually results in distant or faint
breath sounds and decreased chest movement
bilaterally, rather than the differential findings between
the two sides seen in adults.
This infant's circulation does not appear
compromised clinically. The patient was alert with good
pulses and capillary refill. Is this consistent with tension
pneumothorax?
No, the hallmark of tension pneumothorax is
persistent hypoxia (despite supplemental oxygen) with
circulatory compromise (hypotension and/or
bradycardia). The fact that this patient did not have
impaired perfusion should make you refrain from
needling the chest and examine the CXR more carefully.
Re-examine the CXR.
 What at first appears to be a tension pneumothorax
may instead be severe emphysema of one or more
lobes of the lung. Every attempt should be made to
visualize lung markings and the lung edge within the
hyperlucent space. Remember that lung markings
may be very faint because the blood vessels are spread
out. Additionally, there may be reflex hypoxic
vasoconstriction as an attempt to match VQ. Carefully
examining the CXR using a hot light may prevent you
from mistakenly needling the chest and causing a
severe complication. There are indeed lung markings
throughout the left chest (These are evident on the
original film, but it was very difficult to reproduce this on
the scanned image). You decide to intubate the patient
and transfer to the ICU, but the patient's condition
worsens after intubation. What can you do?
If this patient's emphysema becomes life-threatening
(which may happen rapidly if positive pressure is
applied) the only treatment would be a lateral
thoracotomy to allow the lung to herniate out of the
chest. When you call the surgeon, he/she asks if you
are sure this is not hypoplasia of the right lung or
a diaphragmatic hernia. How do you support the
diagnosis of emphysema on CXR?
There are several parameters to assess in order to
answer this question. Before anything else, it is
essential to evaluate the CXR for the presence of any
rotation. A rotated chest film can both mimic and
obscure a mediastinal shift. Evaluation of the clavicles
is one recommended method, but is often confounded
by irregular positioning of both clavicles. Another useful
method is to evaluate the horizontal length of the ribs at
the midchest level measuring from the lateral chest to
the center of the spine on either side. If one side is
longer, the patient is rotated to that side and all
structures will appear to be falsely shifted to the same
side.
View rotated CXR.
What at first appears to be a tension pneumothorax
may instead be severe emphysema of one or more
lobes of the lung. Every attempt should be made to
visualize lung markings and the lung edge within the
hyperlucent space. Remember that lung markings
may be very faint because the blood vessels are spread
out. Additionally, there may be reflex hypoxic
vasoconstriction as an attempt to match VQ. Carefully
examining the CXR using a hot light may prevent you
from mistakenly needling the chest and causing a
severe complication. There are indeed lung markings
throughout the left chest (These are evident on the
original film, but it was very difficult to reproduce this on
the scanned image). You decide to intubate the patient
and transfer to the ICU, but the patient's condition
worsens after intubation. What can you do?
If this patient's emphysema becomes life-threatening
(which may happen rapidly if positive pressure is
applied) the only treatment would be a lateral
thoracotomy to allow the lung to herniate out of the
chest. When you call the surgeon, he/she asks if you
are sure this is not hypoplasia of the right lung or
a diaphragmatic hernia. How do you support the
diagnosis of emphysema on CXR?
There are several parameters to assess in order to
answer this question. Before anything else, it is
essential to evaluate the CXR for the presence of any
rotation. A rotated chest film can both mimic and
obscure a mediastinal shift. Evaluation of the clavicles
is one recommended method, but is often confounded
by irregular positioning of both clavicles. Another useful
method is to evaluate the horizontal length of the ribs at
the midchest level measuring from the lateral chest to
the center of the spine on either side. If one side is
longer, the patient is rotated to that side and all
structures will appear to be falsely shifted to the same
side.
View rotated CXR.
 This neonatal CXR is rotated, as can be determined
by looking at the location of the proximal clavicles and
the non-symmetry of the rib origins. This gives the
CXR the appearance of left sided hyperexpansion with
the heart pushed over to the right; however, this
appearance is purely due to rotational artifact.
Once the degree, if any, of rotation has been
determined, several other areas should be evaluated.
The bony thorax may show increased space between
the ribs on one side, indicative of emphysema or
pneumothorax. The diaphragms should be evaluated
for position and evidence of compression or elevation.
A flattened (compressed) hemidiaphragm implies
emphysema of an adjacent lobe or tension
pneumothorax. An elevated hemidiaphragm implies
volume loss in that hemithorax due to atelectasis,
hypoplasia or a diaphragmatic hernia. A decubitus film
can demonstrate failure of the emphysematous lobe to
deflate when placed down. Fluid in the hemithorax will
displace the heart, but would appear radiopaque.
View patient's CXR again.
This neonatal CXR is rotated, as can be determined
by looking at the location of the proximal clavicles and
the non-symmetry of the rib origins. This gives the
CXR the appearance of left sided hyperexpansion with
the heart pushed over to the right; however, this
appearance is purely due to rotational artifact.
Once the degree, if any, of rotation has been
determined, several other areas should be evaluated.
The bony thorax may show increased space between
the ribs on one side, indicative of emphysema or
pneumothorax. The diaphragms should be evaluated
for position and evidence of compression or elevation.
A flattened (compressed) hemidiaphragm implies
emphysema of an adjacent lobe or tension
pneumothorax. An elevated hemidiaphragm implies
volume loss in that hemithorax due to atelectasis,
hypoplasia or a diaphragmatic hernia. A decubitus film
can demonstrate failure of the emphysematous lobe to
deflate when placed down. Fluid in the hemithorax will
displace the heart, but would appear radiopaque.
View patient's CXR again.
 Our patient's CXR shows:
1. Hyperexpanded left "lung" (actually the left upper
lobe) that herniates into the right chest.
2. Spreading of ribs of the left chest.
3. Shift of the mediastinum to the right.
4. Compression of the left hemidiaphragm.
5. Left lower lobe atelectasis (It is so small, that you
can hardly see it. It is largely obscured.) visible in the
left inferior medial chest.
6. Normal position of the right hemidiaphragm.
7. No infiltrates or fluid.
8. All these findings are consistent with emphysema
of the left upper lobe.
Discussion
An important aspect of pediatric emergency care is
to be aware of congenital anomalies and the manner
and timing with which they present. The differential
diagnosis of any acute medical presentation in the first
few months of life must include congenital problems.
Within the first weeks of life, respiratory and cardiac
problems often present precipitously.
This patient had congenital lobar emphysema of the
left upper lobe and was also found to have a patent
ductus arteriosus. The history suggests mild symptoms
since birth with acute deterioration. At lobectomy, the
left upper lobe bronchus was noted to have
abnormalities of the cartilage structures. The bronchus
was collapsed with an intraluminal mucous plug.
Emphysema may be caused by cartilaginous
malformation, intrinsic obstruction, or extrinsic
compression. This condition is most common in the
upper lobes and associated in 10% of cases with
congenital heart defects, most commonly patent ductus
arteriosus. Most cases present with respiratory distress
within the first 4 months of life and may eventually
require resection. Occasionally, asymptomatic cases
are found fortuitously on chest radiographs in later
years. Evaluation for coexisting congenital anomalies
may be made through non-invasive tests such as
echocardiography, CT, MRI, and ventilation-perfusion
lung scan.
Additional Teaching Points: Be Aware of . . .
Whenever regional emphysema is present in the
lung, suspicion of a foreign body should be very high.
The young age of our patient made this unlikely but in
the high-risk age group, approximately 5 months to 5
years of age, this diagnosis must be pursued even in
the face of a negative history. Often bronchoscopy is
needed to make the diagnosis and alleviate the
condition. Also, think of a foreign body when faced with
cases of recurrent wheezing or pneumonia (See Case
8 of Volume 1, Foreign Body Aspiration in a Child).
If this infant had a true tension pneumothorax,
staphylococcal pneumonia should be highly suspected.
It is most common in the first six months of life and
often has an extremely rapid onset with fever,
tachypnea, and grunting. Commonly, endobronchial
infection ruptures through to the pleural space, creating
a bronchopleural fistula early in the course of disease,
leading to life-threatening pneumothorax and/or
empyema. This requires urgent placement of a chest
tube, along with appropriate antibiotics and treatment
for septic shock. Staphylococcal pneumonia develops
rapidly and initial CXR findings may show no evident
infiltrate or only a smal amount of pleural fluid.
References
Gerbeaux J, Couvreur J, Tournier G. Pediatric
Respiratory Disease, second edition. New York, J.
Wiley and Sons, 1982, pp. 217-223.
Markowitz RI, Mercurio MR, Vahjen GA, Gross I,
Touloukian RT. Congenital Lobar Emphysema.
Clinical Pediatrics 1989;28(1):19-23.
Scarpeli EM, Auld P, Goldman HS. Pulmonary
Disease of the Fetus, Newborn, and Child.
Philadelphia, Lea & Febiger, 1978, pp. 194-196.
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S. Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams &
Wilkins, 1993, pp. 1336-1362.
Our patient's CXR shows:
1. Hyperexpanded left "lung" (actually the left upper
lobe) that herniates into the right chest.
2. Spreading of ribs of the left chest.
3. Shift of the mediastinum to the right.
4. Compression of the left hemidiaphragm.
5. Left lower lobe atelectasis (It is so small, that you
can hardly see it. It is largely obscured.) visible in the
left inferior medial chest.
6. Normal position of the right hemidiaphragm.
7. No infiltrates or fluid.
8. All these findings are consistent with emphysema
of the left upper lobe.
Discussion
An important aspect of pediatric emergency care is
to be aware of congenital anomalies and the manner
and timing with which they present. The differential
diagnosis of any acute medical presentation in the first
few months of life must include congenital problems.
Within the first weeks of life, respiratory and cardiac
problems often present precipitously.
This patient had congenital lobar emphysema of the
left upper lobe and was also found to have a patent
ductus arteriosus. The history suggests mild symptoms
since birth with acute deterioration. At lobectomy, the
left upper lobe bronchus was noted to have
abnormalities of the cartilage structures. The bronchus
was collapsed with an intraluminal mucous plug.
Emphysema may be caused by cartilaginous
malformation, intrinsic obstruction, or extrinsic
compression. This condition is most common in the
upper lobes and associated in 10% of cases with
congenital heart defects, most commonly patent ductus
arteriosus. Most cases present with respiratory distress
within the first 4 months of life and may eventually
require resection. Occasionally, asymptomatic cases
are found fortuitously on chest radiographs in later
years. Evaluation for coexisting congenital anomalies
may be made through non-invasive tests such as
echocardiography, CT, MRI, and ventilation-perfusion
lung scan.
Additional Teaching Points: Be Aware of . . .
Whenever regional emphysema is present in the
lung, suspicion of a foreign body should be very high.
The young age of our patient made this unlikely but in
the high-risk age group, approximately 5 months to 5
years of age, this diagnosis must be pursued even in
the face of a negative history. Often bronchoscopy is
needed to make the diagnosis and alleviate the
condition. Also, think of a foreign body when faced with
cases of recurrent wheezing or pneumonia (See Case
8 of Volume 1, Foreign Body Aspiration in a Child).
If this infant had a true tension pneumothorax,
staphylococcal pneumonia should be highly suspected.
It is most common in the first six months of life and
often has an extremely rapid onset with fever,
tachypnea, and grunting. Commonly, endobronchial
infection ruptures through to the pleural space, creating
a bronchopleural fistula early in the course of disease,
leading to life-threatening pneumothorax and/or
empyema. This requires urgent placement of a chest
tube, along with appropriate antibiotics and treatment
for septic shock. Staphylococcal pneumonia develops
rapidly and initial CXR findings may show no evident
infiltrate or only a smal amount of pleural fluid.
References
Gerbeaux J, Couvreur J, Tournier G. Pediatric
Respiratory Disease, second edition. New York, J.
Wiley and Sons, 1982, pp. 217-223.
Markowitz RI, Mercurio MR, Vahjen GA, Gross I,
Touloukian RT. Congenital Lobar Emphysema.
Clinical Pediatrics 1989;28(1):19-23.
Scarpeli EM, Auld P, Goldman HS. Pulmonary
Disease of the Fetus, Newborn, and Child.
Philadelphia, Lea & Febiger, 1978, pp. 194-196.
Templeton JM. Thoracic Emergencies. In: Fleisher
GR, Ludwig S. Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams &
Wilkins, 1993, pp. 1336-1362.