Foreign Body Aspiration in a Child
Radiology Cases in Pediatric Emergency Medicine
Volume 1, Case 8
Rodney B. Boychuk, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 17 month old male presents to the ED in the
evening with a one-hour history of noisy and abnormal
breathing after a choking episode while he was eating a
chocolate and almond bar. He was able to speak and
drink fluids without difficulty.
Exam: VS T36.8, P200 (crying), R28 (crying),
oxygen saturation 99% in room air. He appeared alert,
with no signs of respiratory distress. He was able to
speak, had no cyanosis, no drooling, and no dyspnea.
His lung sounds showed mild wheezing with possible
mild inspiratory stridor. An albuterol aerosol was
administered but no improvement was noted. A
chest radiograph was ordered.
View CXR.
 Questions:
1. Are any foreign bodies visible on this radiograph?
2. Are there any subtle findings on this radiograph
to suggest a foreign body?
3. Are there other radiologic procedures that can be
done to try to identify a foreign body?
4. Is an invasive procedure necessary or indicated
at this point, i.e., bronchoscopy?
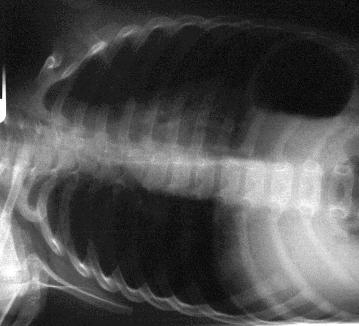
This CXR is within normal limits; however, when a
clinical suspicion of an airway foreign body is present,
a standard PA and lateral CXR are an insufficient
evaluation. A lateral neck film should be obtained to
examine the upper airway for evidence of swelling or
foreign body. Decubitus films and/or expiratory films
should also be obtained to look for evidence of air
trapping.
View supplementary radiographs.
Lateral neck.
Questions:
1. Are any foreign bodies visible on this radiograph?
2. Are there any subtle findings on this radiograph
to suggest a foreign body?
3. Are there other radiologic procedures that can be
done to try to identify a foreign body?
4. Is an invasive procedure necessary or indicated
at this point, i.e., bronchoscopy?
This CXR is within normal limits; however, when a
clinical suspicion of an airway foreign body is present,
a standard PA and lateral CXR are an insufficient
evaluation. A lateral neck film should be obtained to
examine the upper airway for evidence of swelling or
foreign body. Decubitus films and/or expiratory films
should also be obtained to look for evidence of air
trapping.
View supplementary radiographs.
Lateral neck.
 Expiratory Chest.
Expiratory Chest.
 Left lateral decubitus.
Left lateral decubitus.
 Right lateral decubitus.
Right lateral decubitus.
 The lateral neck radiograph is within normal limits.
The black dots in the upper right are pointing to a
metallic object in the holder's watch band.
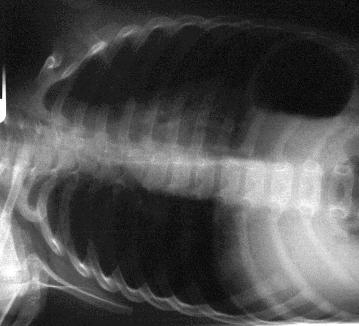
These other radiographs were interpreted as
possible bilateral air trapping.
The expiratory view is fairly symmetric in this
instance. A foreign body in a bronchus is expected to
show air trapping with some hyperexpansion visible in
that lung. In the expiratory view, both lung volumes
should normally be decreased. If one side is still
expanded during expiration, this indicates air trapping
and a possible foreign body on that side.
An expiratory CXR that shows symmetry of both
lung volumes does not rule out a foreign body. Such a
CXR is often assumed to be consistent with asthma.
Although this is often true, this is occasionally a pitfall
that should be avoided by considering such a CXR to
also be consistent with a tracheal foreign body.
Examine the expiratory CXR again. It shows that both
lungs empty poorly, indicating bilateral air trapping.
This could be consistent with asthma or with a tracheal
foreign body.
The left lateral decubitus view (left side down) shows
the left lung volume to be somewhat smaller than the
right lung volume. However, one might expect the left
lung to be even smaller in the dependent position, so
perhaps it isn't as small as it should be. This suggests
some degree of air trapping on the left.
The right lateral decubitus view (right side down)
is of poor quality. The original film was very dark so
the scanned image is very grainy. This shows the right
lung to be clearly expanded even though it is
dependent. This suggests air trapping since a normal
lung should appear smaller in the dependent position.
The patient was taken to the operating room for
bronchoscopy. At bronchoscopy, about 15-20 pieces of
nut particles in the lower trachea and in both major
bronchi were found. They were somewhat difficult to
remove because of their small size. Most were
removed with grasping forceps and suction. He did well
postoperatively.
Discussion and Teaching Points:
Approximately 75% of all cases of foreign body
aspiration occur in children less than 3 years of age.
Organic debris is most frequently retrieved on
bronchoscopy. Peanuts are the most common
offending agent. Unfortunately, only 6-17% of airway
foreign bodies are radio-opaque. Respiratory
symptoms may be produced by an object lodged
anywhere in the airway, from the hypopharynx to a
segmental bronchus.
Children who ingest or aspirate foreign bodies may
present in acute respiratory distress days or months
after the aspiration episode. Between 50% and 90% of
children have a suggestive history, most commonly of
an acute episode of paroxysmal cough. Other common
signs are cyanosis, choking, and dyspnea. However,
delays in presentation for care are common, and
concern about aspiration as a cause of the child's
symptoms may diminish as the primary event becomes
more distant. Only half of all children are diagnosed
correctly in the first 24 hours after an aspiration event.
An additional 30% receive the correct diagnosis in the
following week, while the remainder may have delays in
diagnosis of weeks to years. One-fourth of children
may be asymptomatic at the time of presentation, and
up to 38% may have no helpful physical exam findings.
The complete triad of coughing, wheezing, and
decreased or absent breath sounds is present in only
about 40% of cases. Other suggestive physical exam
findings are stridor, tachypnea, retractions, rales, and
fever. They are often misdiagnosed as croup, asthma,
pneumonia, or bronchitis. This is a diagnostic pitfall
that should be avoided. Thus, the diagnosis of foreign
body aspiration must be considered in any previously
well, child who has a history of acute onset of choking,
coughing, or wheezing, as well as any child who has a
poorly defined, chronic respiratory complaint.
Remember this general principle:
Nuts + Choking = Bronchoscopy
(regardless of radiographic results)
Roughly 85% of foreign bodies are bronchial, while
15% are laryngotracheal. Laryngotracheal foreign
bodies are more difficult to diagnose and they have a
higher mortality rate. Differential findings, clinically or
radiographically, may only be present in unilateral
bronchial foreign bodies. Differential findings are often
absent in bilateral bronchial foreign bodies or
laryngotracheal foreign bodies. Additionally, foreign
bodies may shift in position. Thus, a previously
suspicious radiographic study may be negative if it is
repeated. One cannot assume that such a patient is
now normal since a more likely explanation is that the
foreign body has moved. Avoid this pitfall.
Although appropriate radiologic studies may localize
the site of the foreign body, a significant number of
children with retained airway foreign bodies have
non-diagnostic films. Radiologic evaluation should start
with AP and lateral views of the chest and neck.
Although plain films may be interpreted as normal,
differential inflation of the affected lung, the most
common abnormality identified, may be documented by
fluoroscopy, lateral decubitus views, or an assisted
expiratory film (the examiner compresses the patient's
abdomen during expiration). Other indirect signs of an
airway foreign body include reabsorption atelectasis
beyond the site of bronchial obstruction, and the
presence of pulmonary infiltrates reflecting an
inflammatory reaction. One source (Esclamado)
reported positive findings on chest radiographs in only
42% of children with laryngotracheal (as opposed to
bronchial) foreign bodies, but a higher rate of positive
findings on lateral neck films in the same series. This
emphasizes the need to direct the examination to the
neck (ie., lateral neck view) when signs of upper airway
obstruction are present. Esophageal foreign bodies
may also cause predominantly respiratory symptoms.
Although CT scan, xeroradiography, and
ultrasonography have been advocated for foreign body
imaging, their utility is not well defined at this time.
CT scanning may be non diagnostic because of
respiratory motion (resulting in poor images) and such
patients usually require sedation which can be risky in
the presence of airway compromise. Given the high
morbidity associated with delay in the diagnosis of an
airway foreign body, and the limited sensitivity of
radiographic studies in identifying this condition, clinical
judgment must dictate whether the child should be
scheduled for diagnostic bronchoscopy in the absence
of radiographic findings.
References
Schunk JE. Foreign Body-Ingestion/Aspiration. In:
Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition. Baltimore, Williams
& Wilkins, 1993, pp. 210-217.
Brownstein D. Foreign Bodies of the
Gastrointestinal Tract and Airway. In: Barkin R (ed).
Pediatric Emergency Medicine Concepts and Clinical
Practice. Chicago, Mosby Year Book, 1992, pp.
311-314.
Hamilton AH, Carswell F, Wisheart JD. The Bristol
Children's Experience of Tracheobronchial Foreign
Bodies 1977-87. Bristol Med Chir Journal 1989;104:72.
Esclamado RM, Richardson MA. Laryngotracheal
Foreign Bodies in Children. American Journal of
Diseases in Children 1987;141:259.
The lateral neck radiograph is within normal limits.
The black dots in the upper right are pointing to a
metallic object in the holder's watch band.
These other radiographs were interpreted as
possible bilateral air trapping.
The expiratory view is fairly symmetric in this
instance. A foreign body in a bronchus is expected to
show air trapping with some hyperexpansion visible in
that lung. In the expiratory view, both lung volumes
should normally be decreased. If one side is still
expanded during expiration, this indicates air trapping
and a possible foreign body on that side.
An expiratory CXR that shows symmetry of both
lung volumes does not rule out a foreign body. Such a
CXR is often assumed to be consistent with asthma.
Although this is often true, this is occasionally a pitfall
that should be avoided by considering such a CXR to
also be consistent with a tracheal foreign body.
Examine the expiratory CXR again. It shows that both
lungs empty poorly, indicating bilateral air trapping.
This could be consistent with asthma or with a tracheal
foreign body.
The left lateral decubitus view (left side down) shows
the left lung volume to be somewhat smaller than the
right lung volume. However, one might expect the left
lung to be even smaller in the dependent position, so
perhaps it isn't as small as it should be. This suggests
some degree of air trapping on the left.
The right lateral decubitus view (right side down)
is of poor quality. The original film was very dark so
the scanned image is very grainy. This shows the right
lung to be clearly expanded even though it is
dependent. This suggests air trapping since a normal
lung should appear smaller in the dependent position.
The patient was taken to the operating room for
bronchoscopy. At bronchoscopy, about 15-20 pieces of
nut particles in the lower trachea and in both major
bronchi were found. They were somewhat difficult to
remove because of their small size. Most were
removed with grasping forceps and suction. He did well
postoperatively.
Discussion and Teaching Points:
Approximately 75% of all cases of foreign body
aspiration occur in children less than 3 years of age.
Organic debris is most frequently retrieved on
bronchoscopy. Peanuts are the most common
offending agent. Unfortunately, only 6-17% of airway
foreign bodies are radio-opaque. Respiratory
symptoms may be produced by an object lodged
anywhere in the airway, from the hypopharynx to a
segmental bronchus.
Children who ingest or aspirate foreign bodies may
present in acute respiratory distress days or months
after the aspiration episode. Between 50% and 90% of
children have a suggestive history, most commonly of
an acute episode of paroxysmal cough. Other common
signs are cyanosis, choking, and dyspnea. However,
delays in presentation for care are common, and
concern about aspiration as a cause of the child's
symptoms may diminish as the primary event becomes
more distant. Only half of all children are diagnosed
correctly in the first 24 hours after an aspiration event.
An additional 30% receive the correct diagnosis in the
following week, while the remainder may have delays in
diagnosis of weeks to years. One-fourth of children
may be asymptomatic at the time of presentation, and
up to 38% may have no helpful physical exam findings.
The complete triad of coughing, wheezing, and
decreased or absent breath sounds is present in only
about 40% of cases. Other suggestive physical exam
findings are stridor, tachypnea, retractions, rales, and
fever. They are often misdiagnosed as croup, asthma,
pneumonia, or bronchitis. This is a diagnostic pitfall
that should be avoided. Thus, the diagnosis of foreign
body aspiration must be considered in any previously
well, child who has a history of acute onset of choking,
coughing, or wheezing, as well as any child who has a
poorly defined, chronic respiratory complaint.
Remember this general principle:
Nuts + Choking = Bronchoscopy
(regardless of radiographic results)
Roughly 85% of foreign bodies are bronchial, while
15% are laryngotracheal. Laryngotracheal foreign
bodies are more difficult to diagnose and they have a
higher mortality rate. Differential findings, clinically or
radiographically, may only be present in unilateral
bronchial foreign bodies. Differential findings are often
absent in bilateral bronchial foreign bodies or
laryngotracheal foreign bodies. Additionally, foreign
bodies may shift in position. Thus, a previously
suspicious radiographic study may be negative if it is
repeated. One cannot assume that such a patient is
now normal since a more likely explanation is that the
foreign body has moved. Avoid this pitfall.
Although appropriate radiologic studies may localize
the site of the foreign body, a significant number of
children with retained airway foreign bodies have
non-diagnostic films. Radiologic evaluation should start
with AP and lateral views of the chest and neck.
Although plain films may be interpreted as normal,
differential inflation of the affected lung, the most
common abnormality identified, may be documented by
fluoroscopy, lateral decubitus views, or an assisted
expiratory film (the examiner compresses the patient's
abdomen during expiration). Other indirect signs of an
airway foreign body include reabsorption atelectasis
beyond the site of bronchial obstruction, and the
presence of pulmonary infiltrates reflecting an
inflammatory reaction. One source (Esclamado)
reported positive findings on chest radiographs in only
42% of children with laryngotracheal (as opposed to
bronchial) foreign bodies, but a higher rate of positive
findings on lateral neck films in the same series. This
emphasizes the need to direct the examination to the
neck (ie., lateral neck view) when signs of upper airway
obstruction are present. Esophageal foreign bodies
may also cause predominantly respiratory symptoms.
Although CT scan, xeroradiography, and
ultrasonography have been advocated for foreign body
imaging, their utility is not well defined at this time.
CT scanning may be non diagnostic because of
respiratory motion (resulting in poor images) and such
patients usually require sedation which can be risky in
the presence of airway compromise. Given the high
morbidity associated with delay in the diagnosis of an
airway foreign body, and the limited sensitivity of
radiographic studies in identifying this condition, clinical
judgment must dictate whether the child should be
scheduled for diagnostic bronchoscopy in the absence
of radiographic findings.
References
Schunk JE. Foreign Body-Ingestion/Aspiration. In:
Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition. Baltimore, Williams
& Wilkins, 1993, pp. 210-217.
Brownstein D. Foreign Bodies of the
Gastrointestinal Tract and Airway. In: Barkin R (ed).
Pediatric Emergency Medicine Concepts and Clinical
Practice. Chicago, Mosby Year Book, 1992, pp.
311-314.
Hamilton AH, Carswell F, Wisheart JD. The Bristol
Children's Experience of Tracheobronchial Foreign
Bodies 1977-87. Bristol Med Chir Journal 1989;104:72.
Esclamado RM, Richardson MA. Laryngotracheal
Foreign Bodies in Children. American Journal of
Diseases in Children 1987;141:259.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Questions:
1. Are any foreign bodies visible on this radiograph?
2. Are there any subtle findings on this radiograph
to suggest a foreign body?
3. Are there other radiologic procedures that can be
done to try to identify a foreign body?
4. Is an invasive procedure necessary or indicated
at this point, i.e., bronchoscopy?
This CXR is within normal limits; however, when a
clinical suspicion of an airway foreign body is present,
a standard PA and lateral CXR are an insufficient
evaluation. A lateral neck film should be obtained to
examine the upper airway for evidence of swelling or
foreign body. Decubitus films and/or expiratory films
should also be obtained to look for evidence of air
trapping.
View supplementary radiographs.
Lateral neck.
Questions:
1. Are any foreign bodies visible on this radiograph?
2. Are there any subtle findings on this radiograph
to suggest a foreign body?
3. Are there other radiologic procedures that can be
done to try to identify a foreign body?
4. Is an invasive procedure necessary or indicated
at this point, i.e., bronchoscopy?
This CXR is within normal limits; however, when a
clinical suspicion of an airway foreign body is present,
a standard PA and lateral CXR are an insufficient
evaluation. A lateral neck film should be obtained to
examine the upper airway for evidence of swelling or
foreign body. Decubitus films and/or expiratory films
should also be obtained to look for evidence of air
trapping.
View supplementary radiographs.
Lateral neck.
 Expiratory Chest.
Expiratory Chest.
 Left lateral decubitus.
Left lateral decubitus.
 Right lateral decubitus.
Right lateral decubitus.
 The lateral neck radiograph is within normal limits.
The black dots in the upper right are pointing to a
metallic object in the holder's watch band.
These other radiographs were interpreted as
possible bilateral air trapping.
The expiratory view is fairly symmetric in this
instance. A foreign body in a bronchus is expected to
show air trapping with some hyperexpansion visible in
that lung. In the expiratory view, both lung volumes
should normally be decreased. If one side is still
expanded during expiration, this indicates air trapping
and a possible foreign body on that side.
An expiratory CXR that shows symmetry of both
lung volumes does not rule out a foreign body. Such a
CXR is often assumed to be consistent with asthma.
Although this is often true, this is occasionally a pitfall
that should be avoided by considering such a CXR to
also be consistent with a tracheal foreign body.
Examine the expiratory CXR again. It shows that both
lungs empty poorly, indicating bilateral air trapping.
This could be consistent with asthma or with a tracheal
foreign body.
The left lateral decubitus view (left side down) shows
the left lung volume to be somewhat smaller than the
right lung volume. However, one might expect the left
lung to be even smaller in the dependent position, so
perhaps it isn't as small as it should be. This suggests
some degree of air trapping on the left.
The right lateral decubitus view (right side down)
is of poor quality. The original film was very dark so
the scanned image is very grainy. This shows the right
lung to be clearly expanded even though it is
dependent. This suggests air trapping since a normal
lung should appear smaller in the dependent position.
The patient was taken to the operating room for
bronchoscopy. At bronchoscopy, about 15-20 pieces of
nut particles in the lower trachea and in both major
bronchi were found. They were somewhat difficult to
remove because of their small size. Most were
removed with grasping forceps and suction. He did well
postoperatively.
Discussion and Teaching Points:
Approximately 75% of all cases of foreign body
aspiration occur in children less than 3 years of age.
Organic debris is most frequently retrieved on
bronchoscopy. Peanuts are the most common
offending agent. Unfortunately, only 6-17% of airway
foreign bodies are radio-opaque. Respiratory
symptoms may be produced by an object lodged
anywhere in the airway, from the hypopharynx to a
segmental bronchus.
Children who ingest or aspirate foreign bodies may
present in acute respiratory distress days or months
after the aspiration episode. Between 50% and 90% of
children have a suggestive history, most commonly of
an acute episode of paroxysmal cough. Other common
signs are cyanosis, choking, and dyspnea. However,
delays in presentation for care are common, and
concern about aspiration as a cause of the child's
symptoms may diminish as the primary event becomes
more distant. Only half of all children are diagnosed
correctly in the first 24 hours after an aspiration event.
An additional 30% receive the correct diagnosis in the
following week, while the remainder may have delays in
diagnosis of weeks to years. One-fourth of children
may be asymptomatic at the time of presentation, and
up to 38% may have no helpful physical exam findings.
The complete triad of coughing, wheezing, and
decreased or absent breath sounds is present in only
about 40% of cases. Other suggestive physical exam
findings are stridor, tachypnea, retractions, rales, and
fever. They are often misdiagnosed as croup, asthma,
pneumonia, or bronchitis. This is a diagnostic pitfall
that should be avoided. Thus, the diagnosis of foreign
body aspiration must be considered in any previously
well, child who has a history of acute onset of choking,
coughing, or wheezing, as well as any child who has a
poorly defined, chronic respiratory complaint.
Remember this general principle:
Nuts + Choking = Bronchoscopy
(regardless of radiographic results)
Roughly 85% of foreign bodies are bronchial, while
15% are laryngotracheal. Laryngotracheal foreign
bodies are more difficult to diagnose and they have a
higher mortality rate. Differential findings, clinically or
radiographically, may only be present in unilateral
bronchial foreign bodies. Differential findings are often
absent in bilateral bronchial foreign bodies or
laryngotracheal foreign bodies. Additionally, foreign
bodies may shift in position. Thus, a previously
suspicious radiographic study may be negative if it is
repeated. One cannot assume that such a patient is
now normal since a more likely explanation is that the
foreign body has moved. Avoid this pitfall.
Although appropriate radiologic studies may localize
the site of the foreign body, a significant number of
children with retained airway foreign bodies have
non-diagnostic films. Radiologic evaluation should start
with AP and lateral views of the chest and neck.
Although plain films may be interpreted as normal,
differential inflation of the affected lung, the most
common abnormality identified, may be documented by
fluoroscopy, lateral decubitus views, or an assisted
expiratory film (the examiner compresses the patient's
abdomen during expiration). Other indirect signs of an
airway foreign body include reabsorption atelectasis
beyond the site of bronchial obstruction, and the
presence of pulmonary infiltrates reflecting an
inflammatory reaction. One source (Esclamado)
reported positive findings on chest radiographs in only
42% of children with laryngotracheal (as opposed to
bronchial) foreign bodies, but a higher rate of positive
findings on lateral neck films in the same series. This
emphasizes the need to direct the examination to the
neck (ie., lateral neck view) when signs of upper airway
obstruction are present. Esophageal foreign bodies
may also cause predominantly respiratory symptoms.
Although CT scan, xeroradiography, and
ultrasonography have been advocated for foreign body
imaging, their utility is not well defined at this time.
CT scanning may be non diagnostic because of
respiratory motion (resulting in poor images) and such
patients usually require sedation which can be risky in
the presence of airway compromise. Given the high
morbidity associated with delay in the diagnosis of an
airway foreign body, and the limited sensitivity of
radiographic studies in identifying this condition, clinical
judgment must dictate whether the child should be
scheduled for diagnostic bronchoscopy in the absence
of radiographic findings.
References
Schunk JE. Foreign Body-Ingestion/Aspiration. In:
Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition. Baltimore, Williams
& Wilkins, 1993, pp. 210-217.
Brownstein D. Foreign Bodies of the
Gastrointestinal Tract and Airway. In: Barkin R (ed).
Pediatric Emergency Medicine Concepts and Clinical
Practice. Chicago, Mosby Year Book, 1992, pp.
311-314.
Hamilton AH, Carswell F, Wisheart JD. The Bristol
Children's Experience of Tracheobronchial Foreign
Bodies 1977-87. Bristol Med Chir Journal 1989;104:72.
Esclamado RM, Richardson MA. Laryngotracheal
Foreign Bodies in Children. American Journal of
Diseases in Children 1987;141:259.
The lateral neck radiograph is within normal limits.
The black dots in the upper right are pointing to a
metallic object in the holder's watch band.
These other radiographs were interpreted as
possible bilateral air trapping.
The expiratory view is fairly symmetric in this
instance. A foreign body in a bronchus is expected to
show air trapping with some hyperexpansion visible in
that lung. In the expiratory view, both lung volumes
should normally be decreased. If one side is still
expanded during expiration, this indicates air trapping
and a possible foreign body on that side.
An expiratory CXR that shows symmetry of both
lung volumes does not rule out a foreign body. Such a
CXR is often assumed to be consistent with asthma.
Although this is often true, this is occasionally a pitfall
that should be avoided by considering such a CXR to
also be consistent with a tracheal foreign body.
Examine the expiratory CXR again. It shows that both
lungs empty poorly, indicating bilateral air trapping.
This could be consistent with asthma or with a tracheal
foreign body.
The left lateral decubitus view (left side down) shows
the left lung volume to be somewhat smaller than the
right lung volume. However, one might expect the left
lung to be even smaller in the dependent position, so
perhaps it isn't as small as it should be. This suggests
some degree of air trapping on the left.
The right lateral decubitus view (right side down)
is of poor quality. The original film was very dark so
the scanned image is very grainy. This shows the right
lung to be clearly expanded even though it is
dependent. This suggests air trapping since a normal
lung should appear smaller in the dependent position.
The patient was taken to the operating room for
bronchoscopy. At bronchoscopy, about 15-20 pieces of
nut particles in the lower trachea and in both major
bronchi were found. They were somewhat difficult to
remove because of their small size. Most were
removed with grasping forceps and suction. He did well
postoperatively.
Discussion and Teaching Points:
Approximately 75% of all cases of foreign body
aspiration occur in children less than 3 years of age.
Organic debris is most frequently retrieved on
bronchoscopy. Peanuts are the most common
offending agent. Unfortunately, only 6-17% of airway
foreign bodies are radio-opaque. Respiratory
symptoms may be produced by an object lodged
anywhere in the airway, from the hypopharynx to a
segmental bronchus.
Children who ingest or aspirate foreign bodies may
present in acute respiratory distress days or months
after the aspiration episode. Between 50% and 90% of
children have a suggestive history, most commonly of
an acute episode of paroxysmal cough. Other common
signs are cyanosis, choking, and dyspnea. However,
delays in presentation for care are common, and
concern about aspiration as a cause of the child's
symptoms may diminish as the primary event becomes
more distant. Only half of all children are diagnosed
correctly in the first 24 hours after an aspiration event.
An additional 30% receive the correct diagnosis in the
following week, while the remainder may have delays in
diagnosis of weeks to years. One-fourth of children
may be asymptomatic at the time of presentation, and
up to 38% may have no helpful physical exam findings.
The complete triad of coughing, wheezing, and
decreased or absent breath sounds is present in only
about 40% of cases. Other suggestive physical exam
findings are stridor, tachypnea, retractions, rales, and
fever. They are often misdiagnosed as croup, asthma,
pneumonia, or bronchitis. This is a diagnostic pitfall
that should be avoided. Thus, the diagnosis of foreign
body aspiration must be considered in any previously
well, child who has a history of acute onset of choking,
coughing, or wheezing, as well as any child who has a
poorly defined, chronic respiratory complaint.
Remember this general principle:
Nuts + Choking = Bronchoscopy
(regardless of radiographic results)
Roughly 85% of foreign bodies are bronchial, while
15% are laryngotracheal. Laryngotracheal foreign
bodies are more difficult to diagnose and they have a
higher mortality rate. Differential findings, clinically or
radiographically, may only be present in unilateral
bronchial foreign bodies. Differential findings are often
absent in bilateral bronchial foreign bodies or
laryngotracheal foreign bodies. Additionally, foreign
bodies may shift in position. Thus, a previously
suspicious radiographic study may be negative if it is
repeated. One cannot assume that such a patient is
now normal since a more likely explanation is that the
foreign body has moved. Avoid this pitfall.
Although appropriate radiologic studies may localize
the site of the foreign body, a significant number of
children with retained airway foreign bodies have
non-diagnostic films. Radiologic evaluation should start
with AP and lateral views of the chest and neck.
Although plain films may be interpreted as normal,
differential inflation of the affected lung, the most
common abnormality identified, may be documented by
fluoroscopy, lateral decubitus views, or an assisted
expiratory film (the examiner compresses the patient's
abdomen during expiration). Other indirect signs of an
airway foreign body include reabsorption atelectasis
beyond the site of bronchial obstruction, and the
presence of pulmonary infiltrates reflecting an
inflammatory reaction. One source (Esclamado)
reported positive findings on chest radiographs in only
42% of children with laryngotracheal (as opposed to
bronchial) foreign bodies, but a higher rate of positive
findings on lateral neck films in the same series. This
emphasizes the need to direct the examination to the
neck (ie., lateral neck view) when signs of upper airway
obstruction are present. Esophageal foreign bodies
may also cause predominantly respiratory symptoms.
Although CT scan, xeroradiography, and
ultrasonography have been advocated for foreign body
imaging, their utility is not well defined at this time.
CT scanning may be non diagnostic because of
respiratory motion (resulting in poor images) and such
patients usually require sedation which can be risky in
the presence of airway compromise. Given the high
morbidity associated with delay in the diagnosis of an
airway foreign body, and the limited sensitivity of
radiographic studies in identifying this condition, clinical
judgment must dictate whether the child should be
scheduled for diagnostic bronchoscopy in the absence
of radiographic findings.
References
Schunk JE. Foreign Body-Ingestion/Aspiration. In:
Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition. Baltimore, Williams
& Wilkins, 1993, pp. 210-217.
Brownstein D. Foreign Bodies of the
Gastrointestinal Tract and Airway. In: Barkin R (ed).
Pediatric Emergency Medicine Concepts and Clinical
Practice. Chicago, Mosby Year Book, 1992, pp.
311-314.
Hamilton AH, Carswell F, Wisheart JD. The Bristol
Children's Experience of Tracheobronchial Foreign
Bodies 1977-87. Bristol Med Chir Journal 1989;104:72.
Esclamado RM, Richardson MA. Laryngotracheal
Foreign Bodies in Children. American Journal of
Diseases in Children 1987;141:259.