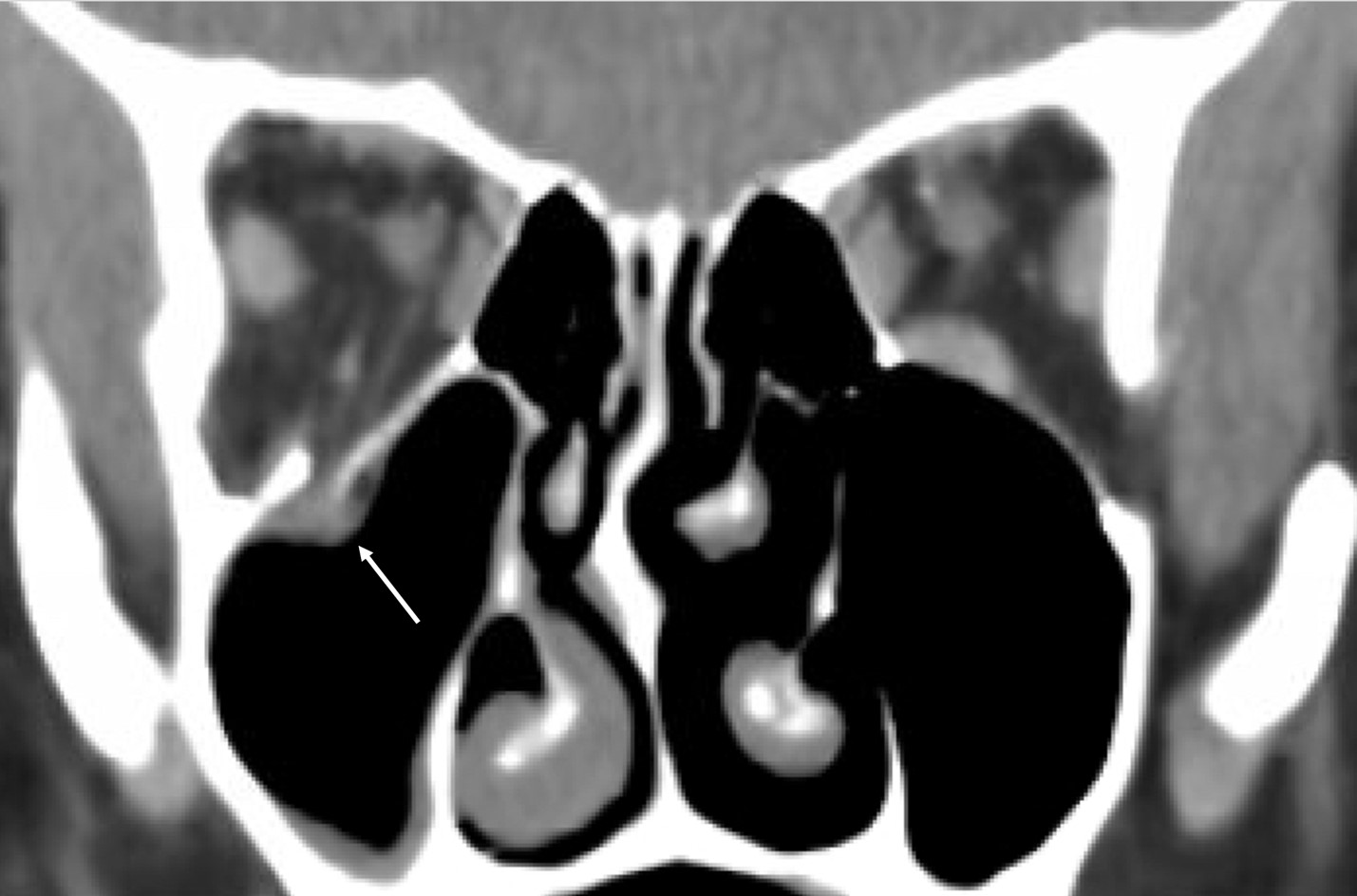
Figure 1. CT scan of a right orbital floor blowout fracture showing a minimally displaced orbital floor and an entrapped inferior rectus muscle (arrow).

An 8 year old male presents to the emergency department with left eye pain, blurry vision, and nausea for the past 2 hours. His mother reports that he had been playing street hockey with his older brother, who accidentally shot a puck that struck the patient in the eye. He has vomited once since being struck. The patient complains of severe pain and states that he canít see. He had been in good health until this incident and is not on any medications.
Exam: VS T 37.6, P 70, RR 18, BP 98/71. He is in severe distress, crying and holding his left eye. His vision is 20/20 in the right eye and 20/30 in the left eye. He is mostly unable to cooperate with extraocular movements due to pain, which is especially severe on superior gaze. No hyphema is visible. There is no evidence of hemorrhage or periorbital ecchymoses.
A CT scan of the orbits is obtained which reveals a left trapdoor fracture of the orbital floor with entrapment of the inferior rectus muscle. An oculoplastic surgeon is consulted and immediate operative reduction and repair is performed (with placement of a nylon foil orbital implant to prevent re-entrapment). Post-surgery, the patientís vision steadily improves and extraocular movements are full.
The orbit refers to the bony portion of the skull that contains the eyeball, lacrimal system, extraocular muscles, nerves (including cranial nerves II-VI), vasculature, and orbital fat. Seven bones make up the orbit: the sphenoid, frontal, zygomatic, ethmoid, lacrimal, maxilla, and palatine bones (1). Orbital fractures represent about 10% to 25% of all facial fractures and are most commonly due to motor vehicle accidents, assaults, falls, and sports related injuries (2,3). Fractures are often categorized by their location at the orbital floor, medial wall, roof, lateral wall, orbital rim, or as part of a zygomaticomaxillary complex (ZMC) fracture (4). With orbital fractures, any potential damage to the globe, extraocular muscles, and optic nerve must be investigated (2). Orbital hemorrhage and intraorbital foreign bodies can also occur with orbital trauma (3).
Common clinical signs in orbital fractures include subconjunctival hemorrhage and periorbital ecchymoses. In the pediatric population particularly, the absence of these signs does not exclude an orbital fracture. Specifically, up to 43% of pediatric orbital fractures do not have visible signs and may require a mobility examination to uncover evidence of fracture (2). Other signs of orbital fracture include diplopia, blurry vision, pain or nausea with eye movement, orbital crepitus, and paresthesia of the cheek, nose, or teeth in the V2 distribution (3-6). Patients with a suspected orbital fracture should ideally be evaluated by an ophthalmologist/oculoplastic surgeon and possibly by an additional facial trauma specialist, such as a plastic surgeon, ENT, or oral and maxillofacial surgery (OMFS) specialist, but these specialists are often not readily available in the emergency department where most of these injuries present. Most mild orbital floor fractures without muscle entrapment are managed without surgery. The diagnosis is confirmed by an orbital CT without contrast, which can identify the fracture location and any entrapment of orbital structures. If more extensive facial fractures are suspected, a CT face without contrast can be ordered with fine cuts and 3D reconstructions (3,5). Yet injuries suspected to simple uncomplicated orbital floor fractures do not necessarily require a CT scan since this exposes children and their developing brains to significant X-ray radiation doses.
Orbital floor fractures can present as a blowout fracture or a trapdoor fracture. Blowout fractures are the most common and occur when transmitted forces increase intraorbital pressure, which is transferred to the thin orbital floor or medial wall. Blowout of the orbital floor can lead to the entrapment of orbital tissue and the inferior rectus muscle. In children and teenagers, extraocular muscle entrapment in a blowout fracture presenting without orbital soft tissue signs is termed as a "white-eyed blowout fracture" (non-ecchymotic). Trapdoor fractures are seen more commonly in pediatric patients compared to adults due to young patientsí highly elastic bone that is more likely to greenstick, spring back into position, and trap the inferior rectus muscle. Restriction and pain in superior and inferior gaze should raise high suspicion for inferior rectus muscle entrapment. In rare cases, muscle entrapment can cause the oculocardiac reflex, where patients experience bradycardia, heart block, nausea, and syncope when attempting extraocular movements. The oculocardiac reflex, along with the risk of extraocular muscle vascular compromise and necrosis, requires immediate operative reduction. Other indications for surgical repair include pain with eye movements, noticeable enophthalmos (the globe is deeper into the orbit), hypoglobus (the globe is more inferior in the orbit), diplopia in primary or downward gaze, and involvement of the more than 50% of the orbital floor with significant orbital volume expansion or tissue prolapse (2,4-7).
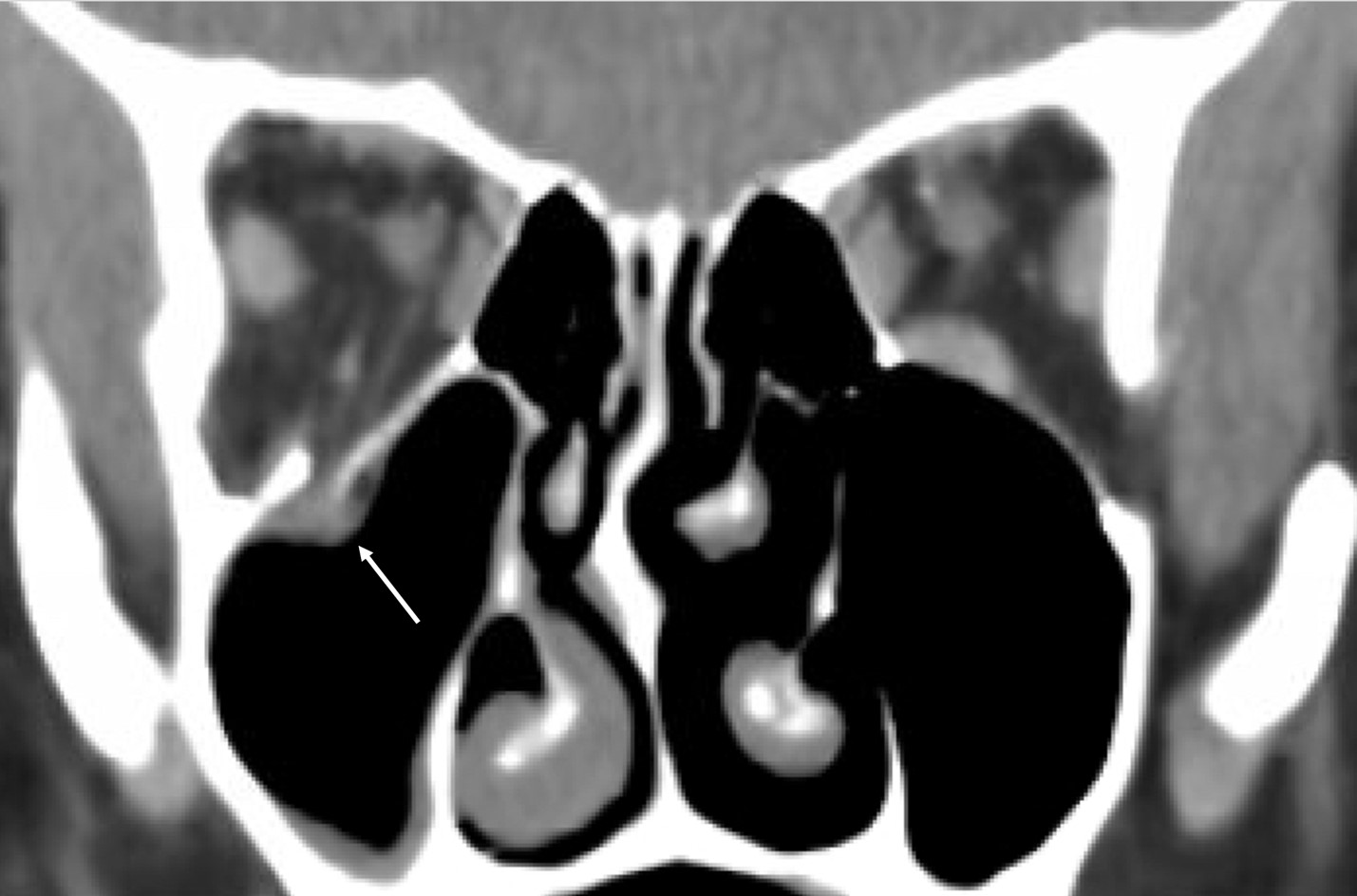
Figure 1. CT scan of a right orbital floor blowout fracture showing a minimally displaced orbital floor and an entrapped inferior rectus muscle (arrow).
Figure 2. CT scan of a left orbital floor blowout fracture showing a minimally displaced orbital floor and an entrapped inferior rectus muscle (arrow).
Medial orbital wall fractures are the second most common due to the fragile, thin bone separating the orbit from the ethmoid sinuses called the lamina papyracea. Fracture to this bone can create a pathway to the nares and ethmoid air cells, resulting in orbital emphysema. Nose blowing can result in copious amounts of air blown into the orbit (orbital emphysema) which can cause intraorbital vascular compromise and loss of vision. Patients should be instructed to not blow their nose to avoid causing orbital emphysema and optic nerve compression. Telecanthus, a widening of the distance between the medial canthi without change in the outer canthal distance, can occur due to involvement of the medial canthal tendon in a naso-orbito-ethmoid (NOE) fracture. Since the medial canthal tendon encases the nasolacrimal sac, tear outflow obstruction can be seen in severe cases. Intraorbital hemorrhage and orbital compartment syndrome can occur from injury to the anterior and posterior ethmoidal arteries, which traverse the medial wall. Indications for surgical repair are similar to those in orbital floor fractures, including entrapment of the medial rectus muscle and enophthalmos (2,4,6).
Orbital roof fractures rarely occur in adults but are more common in the pediatric population. Specifically, fractures of the orbital roof are mostly seen in children younger than 5 years of age, prior to pneumatization of the frontal sinuses. Entrapment of the superior rectus and superior oblique muscles can occur. Orbital roof fractures have a high association with neurologic injury (57% to 90%), including pneumocephalus, dural tears, and cerebrospinal fluid (CSF) leaks. Therefore, neurosurgical consultation should be considered. Coordination with neurosurgery is also needed in some cases complicated by a "growing skull fracture", where fractured bone fragments continue to separate due to growth of the pediatric skull. However, in the absence of extraocular muscle entrapment, diplopia, or CSF leak, nondisplaced roof fractures can be managed without surgical intervention (2,4,7).
Lateral orbital wall fractures usually present as part of a larger fracture, such as with a fracture of the ZMC or the orbital rim. This can occur after a lateral blow to the upper third of the face. Fractures of the orbital rim may have palpable step-offs and may involve the V2 branch of the trigeminal nerve. These fractures often require surgical intervention. Without surgery, the side of the face can begin to flatten and widen, the lateral canthal tendon can be displaced, and exophthalmos or enophthalmos can occur (2,4).
In orbital fractures that do not require immediate surgical repair, surgery can be delayed for 1 to 2 weeks to allow for resolution of orbital edema and a decrease in intraorbital pressure. Conservative management includes placing ice on the orbit and elevating the bed for the first 1 to 2 days. In fractures that expose the orbit to the sinus cavity, broad-spectrum antibiotics can be used for 14 days; however their impact on outcomes is inconclusive (2,6). For some patients, oral corticosteroids can be used for 7 days to decrease risk of diplopia and mobility restricting edema (3). Studies have shown that late orbital fracture repair performed months to years after the injury can also have excellent results with improvement in extraocular mobility, enophthalmos, and hypoglobus (8).
Orbital hemorrhage can present either in conjunction with an orbital fracture or separately after trauma to the head or face. It is more commonly seen in patients who are on anticoagulant or antiplatelet medications. Since the orbit is a confined, bony structure with limited ability to expand, hemorrhage can lead to orbital compartment syndrome, which is vision-threatening. Increasing pressure within the orbit can rapidly compress the optic nerve and retina, resulting in ocular and nerve ischemia. Signs of orbital hemorrhage include decreased vision, inability to open the eyelids, presence of a relative afferent pupillary defect (RAPD), increased intraocular pressure (IOP), decreased ocular movement, and proptosis of the eye. Optic disc swelling and vascular occlusion may be present on fundoscopy. Orbital hemorrhage is a clinical diagnosis and imaging with CT orbits should only be performed in patients without highly worrisome signs (e.g. RAPD or decreased vision) who do not need emergent treatment. Ophthalmology should be consulted and the head of the bed should be elevated. Coughing and straining should be avoided to prevent any further increases in IOP. Patients without increased IOP, mild hemorrhage, and no alarming symptoms suggesting compartment syndrome may be monitored. In patients with increased IOP but no orbital signs, IOP lowering medications such as topical beta-blockers, alpha-agonists, or carbonic anhydrase inhibitors can be considered. In patients who are concerning for ocular ischemia, optic neuropathy, or orbital compartment syndrome, emergent lateral canthotomy and cantholysis or a full-thickness lid split should be conducted within 120 minutes to optimize visual recovery (3,5).
Intraorbital foreign bodies can occur in children from falls, or from higher velocity trauma such as gunshots or explosions. Loss of vision is a common presentation either from the direct trauma or from a resulting infection. CT scan is the imaging modality of choice in most cases, especially if the foreign body is suspected to be metal. MRI is superior in cases where the foreign body is an organic material such as wood. Metallic foreign bodies containing copper, iron, and lead must undergo surgical removal due to possible inflammatory reaction, retinal toxicity, and ocular damage. Organic materials require urgent surgical exploration and removal of the foreign body since they predispose to orbital infections. The decision to surgically remove an intraorbital foreign body ultimately depends on the location and type of material. Foreign bodies located more posteriorly may be managed conservatively due to the high risk of removal. Removing wood is also difficult due to the high chance of fragmentation, and even the smallest pieces can cause infection (3,5,6).
Questions
1. Name the seven bones that make up the orbit.
2. True/False: Almost all cases of pediatric orbital fractures will present with subconjunctival hemorrhage and/or periorbital ecchymoses.
3. A 6 year-old male presents after being struck in the right eye resulting in pain and nausea. He is found to be bradycardic and has an episode of syncope when attempting extraocular movements. What should be suspected and what is the immediate next step?
4. A 7 year old female presents to the emergency department after sustaining head trauma. On exam she has a relative afferent pupillary defect (RAPD), increased intraocular pressure (IOP), and proptosis of the eye. What should be suspected and what is the immediate next step?
5. A 15 year old male presents with an intraorbital foreign body composed of wood. What is the appropriate imaging modality of choice and a possible complication?
References
1. Cornelius CP, Probst F, Metzger MC, et al. Anatomy of the Orbits. In: Dubois L, Becking AG, Fernandes RP (eds). Atlas of the Oral and Maxillofacial Surgery Clinics of North America. 2021;29(1):1-18. Elsevier, Philadelphia. https://doi.org/10.1016/j.cxom.2020.11.001
2. Roth FS, Koshy JC, Goldberg JS, et al. Pearls of orbital trauma management. Semin Plast Surg. 2010;24(4):398-410. doi: 10.1055/s-0030-1269769.
3. Gordon AA, Tran LT, Phelps PO. Eyelid and orbital trauma for the primary care physician. Dis Mon. 2020;66(10):101045. doi: 10.1016/j.disamonth.2020.101045.
4. Lozada KN, Cleveland PW, Smith JE. Orbital Trauma. Semin Plast Surg. 2019;33(2):106-113. doi: 10.1055/s-0039-1685477.
5. Pargament J, Correa ZM, Augsburger JJ. Chapter 19. Ophthalmic Trauma. In: Riordan-Eva P, Augsburger JJ (eds). Vaughan & Asbury's General Ophthalmology, 19th edition. 2018. McGraw Hill, New York. pp:1-17.
6. Olitsky SE, Marsh JD. Chapter 653. Injuries to the Eye. In: Kliegman RM, St. Geme JW, Blum NJ, et al (eds). Nelson Textbook of Pediatrics, 21st edition. 2020. Elsevier, Philadelphia. pp: 3393-3397.
7. Parameswaran A, Marimuthu M, Panwar S. Chapter 57. Orbital Fractures. In: Bonanthaya K, Panneerselvam E, Manuel S, et al (eds). Oral and Maxillofacial Surgery for the Clinician. 2021. Springer, Singapore. pp: 1201-1250.
8. Scawn RL, Lim LH, Whipple KM, et al. Outcomes of Orbital Blow-Out Fracture Repair Performed Beyond 6 Weeks After Injury. Ophthalmic Plast Reconstr Surg. 2016;32(4):296-301. doi: 10.1097/IOP.0000000000000511.
Answers to questions
1. The orbit is made up of the sphenoid, frontal, zygomatic, ethmoid, lacrimal, maxilla, and palatine bones.
2. False. 43% of pediatric orbital fractures do not have visible signs such as subconjunctival hemorrhage or periorbital ecchymoses. Specifically in children, extraocular muscle entrapment in a blowout fracture without external visible signs is termed as a "white-eyed blowout fracture". Therefore, a motility examination may be required to uncover an orbital fracture.
3. There should be high suspicion for an oculocardiac reflex in this patient, where there is bradycardia, heart block, nausea, and syncope when attempting extraocular movements due to muscle entrapment. This requires immediate ophthalmic operative reduction.
4. There should be a high suspicion for orbital compartment syndrome, which can occur due to hemorrhage in the confined orbital space. This can rapidly compress the optic nerve and retina, and is vision-threatening. Emergent decompression with lateral canthotomy must be conducted within 120 minutes to optimize visual recovery.
5. For intraorbial foreign bodies composed of organic materials like wood, MRI is the imaging modality of choice. Organic materials predispose to orbital infection, and therefore require urgent surgical exploration.